|
This week I was faced with a question that prompted reflection on our early days as a newly diagnosed Type 1 Diabetic family (6 years ago). I have always felt like I existed in this time in the hospital in a haze, with information spewing around me and there I sat on Harrison's hospital bed, trying to internalise it all and make sure I knew what I needed to know to keep my son alive. We bought a notebook and everything the Dr explained was feverishly written down: "Notes on how to keep our son alive".
Imagine writing the hardest exam of your life, only, while you are doing so you are also processing the near loss of your child, and his ultimate diagnosis with a Type 1 Diabetes. It is up to you to pass this exam under these conditions, and to do so with flying colours because the alternate could be fatal. We were lucky to have received our education from a specialist in the field and there are many who are not given this opportunity and are almost left to their own devices to take care of themselves with this disease that they have barely had an education on. Heart breaking to dwell on this uncertainty after as big a diagnosis as Diabetes - whether it is Type 1 or Type 2. Can you imagine the most important education of your life - can you imagine needing this education and just not getting it at all? A few weeks out of hospital and I began my journey of sharing our diagnosis story, and the things that we have learned along the way. It's always been ingrained in me to capitalise on the opportunities life throws at us - whether they're good or bad lemons. My heart was always set on creating educational material that would adequately help newly diagnosed families of young children navigate these early days especially: A glossary of words explaining some of the terminology, carb counting 101, what I like to call the diabetes triangle which is my explanation for the relationship between carbs, glucose and insulin... There are many diagrams and illustrations in my mind that help explain difficult concepts in easy ways. Perhaps there is still an opportunity here who knows. All I need is time and a big corp that is willing to fund the rest. I think the hardest lesson as a caregiver of a Type 1 Diabetic is not to let go of your own self. Your children are your priority after all, but that doesn't mean you sacrifice all of you. They still need you at the end of the day. So it is important to make sure you are looking after yourself and that you set yourself up with the support system you need to make it out alive as much as your child needs to. Those words are easy to say - hard to put into practice. I can understand that. You probably have a list of things that you wish you had learned in the very early days of diagnosis... Leave a comment or email me hello@typeonewarrior.co.za - I'd love to compile and share with our fellow T1 families.
0 Comments
Hi everyone. Candice here. It's been a little while! 2023 is well underway and both Megan (our Warrior Dietitian) and I feel like we are treading water catching our breaths.
This is a topic of conversation that plays through my mind often. For those who know us, we have two sons, Harrison and Lincoln. Harrison, now 7, was diagnosed at 11 months old with Type 1 Diabetes and his little brother Lincoln, now 4 years old, has thus far escaped the autoimmune disease. That's not to say that we haven't had our scares where Rowan and I have finger prick tested him just to suss out the BG levels. I'm currently enrolled in a Diabetes Advocacy course and in one of our modules the topic of statistics comes up... And the thing about these "numbers" for me is I have always found their effect quite minimising of the disease (any disease for that matter), especially with first-hand experience of the disease. I want to touch on one of my discussion points because it has played on my mind since I found out I was pregnant with my second son, Lincoln. I think as a parent of a type one child, "statistics" or "numbers" have become somewhat of a misnomer for me. Neither my husband nor I have type 1 diabetes and it isn't in our family. Before Harrison was diagnosed, statistically, his chances of getting Type 1 Diabetes was 0,4%. A number we didn't really blink an eyelid at. It works out to 1 in every 250 I think (creative brain - not mathematical brain). Those odds seem unlikely in your favour, especially because it's not in the family. Right? Well, with my second son now, Lincoln, given that his sibling is a type 1 diabetic, his chance of becoming one himself has increased from that of 0,4% to a much greater 5%, which works out to 1 in 20. Was it just me or did that frighten you too...? When I internalised the jump of 0,4% to 5% chance, I couldn't help but feel the paddle pool get a whole lot smaller! We have lived with Diabetes for over 6 years in our family now and with time I have learned some things to help me get over, or better manage, that fear of a potential diagnosis in Lincoln. When I talk to friends and family I am always encouraged and urged to share and so today I thought I would jump in with a summary of some advice from me, a fellow Type One Warrior parent, on getting over that fear of a potential diagnosis in a second child. "Getting over" (I hate those words) the fear of a potential second diagnosis in your family can be challenging but below are some steps that could help navigate and manage those worrisome thoughts a little better. 1. Diabetes 101 - learn everything you can about Type 1 Diabetes. The better your understanding of the disease, its causes, and its treatments, can help dispel misconceptions and reduce the fear of another diagnosis. That old saying "forewarned is forearmed" might not be the best here but it comes to mind because you are already in the thick of it. As you provide your Type 1 Diabetic child with the best care, it will only stand you in even better stead for in case your second child is ever diagnosed. 2. Find that support system - talking to a healthcare professional, finding a support group, or even turning to a loved one you can help you process your emotions and feel less alone in your worries. We might not like to talk about it - this is very hard for me - but those things that worry you are sometimes better when they're aired. 3. Don't forget to look after yourself! This is a big one, and boy have I struggled with this. Taking care of your mental and physical health through activities like exercise, mindfulness, and healthy eating is proven to have a positive effect on your overall wellbeing and also helps reduce anxiety. The trick is to get to this point. We so often choose the path of personal neglect and unfortunately this leads you down the slippery slope of caregiver burnout faster than you can imagine. Start with small things - little pockets of time you can allocate yourself to check-in and assess where you need to practice a little self-care. 4. How about turning that frown upside down... How about reframing those statistics that weigh you down and looking at the positives? Lincoln might have a 4% chance of becoming a Type 1 Diabetic, but he also has a 96% chance that it may never happen. It can be hard to reframe but focus on the positive aspects of life and the things that you can control! 5. Ultimately you want to live in the present and focus on what is happening now... not what "might happen". Deep-rooted fears and worries might require more therapy to help you worry less about the possibility your second child will be diagnosed. And there is nothing wrong with therapy. We cannot change or control the outcome so the best advice I'd offer another parent with these worries would be to live as meaningful a life as possible because a potential diagnosis won't change the outcome, and it is still possible to live a fulfilling life regardless of your health status.
For the past few weeks, Zahni and I have been exchanging many an email and message working on an upcoming collaboration that we simply cannot wait to reveal. I feel honoured to have had Zahni contribute to this particular feature - getting really deep on certain topics. I hope you enjoy reading her story as much as I did hearing it.
Before we dive right in I just wanted to remind everyone that there are no two journeys the same and it's for this very reason that we like to share these features. It's to show all of us that the Type One Diabetes diagnosis is not specific to any one type of person. There is no discrimination and is unpredictable to say the least. There will be struggles along the way, and so too will there be triumphs.
Your diagnosis story
I would first have to go back about two weeks before I was diagnosed. They broke into our house and I woke up with the burglar still in the house. It was very traumatic and it was said that the shock caused me to become a diabetic. 2 weeks after the incident I started showing the usual diabetes symptoms. I was very thirsty, irritable and also lost a lot of weight. I remember visiting my father for the weekend and having an accident in my bed. He forbade me to drink anything after 7pm and I remember sneaking to the kitchen to get more water. There is a difference between being thirsty and having the diabetes thirst. Trust me. I went home the next day and my father told my mom that I was sick and acting strange. The next morning we went to the Dr. I was in my school dress thinking I would go back to school after the appointment, thinking it was only a bladder infection. They tested my sugar and it was extremely high. The Dr told us to go straight to the ER. I was so scared as no one was really talking to me or explaining what was going on. At the hospital they tried to force me to sit in a wheel chair, which I refused. I later realised that the wheel chair might have been my best chance of escaping. What do you do for a living? I studied Theology at Stellenbosch University, but after I was blessed with my daughter, I decided to use my degree to pursue another profession. I started teaching English online and that is currently still my full time job. I also started Sweetner Diabetes Accessories. The main purpose of Sweetner was to help afford my own CGM's, but it blew up to such an extent that I can now give back and help others as well. I am so extremely blessed with all the support I have received. I am also available to the parents if they need any advice or just need to vent a bit. I love having a personal relationship with each of my clients. I am hoping to grow Sweetner even more by adding new and affordable products every week. Diabetics have enough expenses already, making life a bit sweeter should not be another financial burden. I love making the orders feel like little gifts and not just more medical equipment. Sweetner really does make life sweeter. Noteable Hypoglycaemic Moments I have had more Hypo’s than your average diabetic, but I do not remember most of them. My mom recalled one time where I had a low at 3am and managed to call her to my room. When she got there my phone was covered in blood because I was trying to test my sugar on my phone screen. More recently I “came to” on the kitchen floor in front of my toddlers sweets drawer. She was not impressed with the damage I had done. I got and still get most of my hypo’s in the middle of the night. I would have snacks next to my bed, but by the time I wake up, I cannot reach for it. Those are the worst. A Funny High Moment This isn’t a hypo story, but rather a funny high story. When my sugar goes up, I get this “confidence”. Similar to being a bit tipsy. I got the courage to speak to a boy that I liked in Grade 9. He ended up asking me to go see a movie. I was super excited. The day we went to see the movie, he asked me what was wrong. Nothing was wrong, my sugar was just not high enough for me to not be my introvert shy self. So, I explained to him… He got up and went to go buy me smarties. I do not think he realised how much that had an impact on my little 15 year old heart and self esteem. But still, funny if I think about it now. As a child/teenager, were you confident in your diagnosis or did you have moments of feeling ashamed? I wouldn’t say I was ashamed, but I was in denial. The doctors used to tell my parents that I have not accepted my diagnoses. I did not want to be different or stand out in any way. I would sit in a class and go low, because I did not want to be the only one eating in class. I would go low during a test, but try to power through it, because I did not enjoy the mean comments from my classmates calling me out for “faking” to get out of a test. I loved learning, even at university, still do. So I would prepare everything to be able to study and then comes test day and my sugar goes completely “whack” because of stress and I end up not being able to write. It’s really unfair.
What was the most difficult thing to overcome when you were first diagnosed, and how do you feel now about the same?
When I was younger, I think the biggest obstacle was letting go of some of my favourite foods. We did not do carb-counting back then and worked according to a sliding scale. All sugary and yummy foods were out and I was forced to eat a lot more than I wanted to. As I got older and technology improved, carb-counting became a thing and diabetics aren’t as restricted with food as back then. It really is great to be able to eat whatever I like, but everything in moderation of course. I like having control over the carbs I eat and having the knowledge to carb count.
In the above story shared on Facebook, Zahni goes into detail about how a culture of fear is shaped amongst Diabetics with the likes of Diabetic posters that show a skewed outlook for all the negative implications of the disease.
Navigating school/work place with T1D? Before my insulin pump, Diabetes completely took over my life. I was not anything other than my diabetes. I missed a lot of school, was constantly feeling sick and could not get anything done. Starting the grown up life, my diabetes management did not improve, only difference was, I had to do the things that had to be done, regardless of how I felt. Now, with the insulin pump, diabetes feels like only a small part of my life. It is just something I get to live with. I no longer struggle with everyday tasks and I have more energy to be the best person and mom I can be. There are bad days, as with everyone, but my life quality has certainly improved the last 2 months.
Most annoying things people have said about your Type 1 Diabetes:
I wouldn’t say it is annoying, but rather that a lot of people do not educate themselves over the proper care and protocol when it comes to a diabetic in need. I had an anxiety attack a few weeks ago. I was sitting in the back of my car, trying to calm myself. A very sweet lady saw that I was struggling and came over to help. My friend told her that I am a diabetic and that I was feeling anxious. She immediately starting shouting that I need sugar. I tried to gesture that my sugar is not low, and my friend even told her that my sugar levels are fine, but she was adamant that I need sugar. She even called first aid at the mall to come give me sugar. I understand that she was trying to help and I am extremely grateful, but had they given me sugar, it would have made things so much worse. I read that around 4,5 million people in SA has diabetes (type 2 included). Surely there must be a way to share the proper information. Share, share, share, we are everywhere! What are your common hypo symptoms, if you can feel a low coming on? My legs go numb. I also start feeling sweaty and anxious. Favourite hypo snack I love green Fizzers. I also sometimes have a few sips of Steri Stumpi. My favourite go-to is regular Coke. I think it might be a head thing as well, but I just feel more at ease when drinking a bit of coke to fix a hypo. Also, super c’s. What do you do to stay active? Before two months ago, I did the bare minimum. Most days I did not have energy to get out of bed, let alone exercise. But, having better control over my levels now had given me the opportunity to start getting active again. I came into the habit of going to the gym every morning. Some days are better than others. Even if I cannot do a full workout every day, I still go to keep myself motivated.
Best part about being type 1
Diabetes taught me very important life skills. I can multi task and plan ahead. It helps we stay organised, for the most part, and forced me to grow up a bit sooner than I would have liked. In the end, it made the person I am today. Unfortunately stressed for the most part and filled with anxiety, but I get things done and I work very hard to achieve my goals. Hardest part about being type 1 The hardest part must be when you have plans and things need to get done, but your body is just failing you. You go low, or you go high or you are still recovering from a low or high. All of the above. I have always been a worrier and I would stress my sugar to the 30’s. I remember entering a debate competition in gr7, winning, but having to be rushed to the hospital in DKA straight after. Tests, deadlines, anything remotely stressful would turn me into Snoop Dog. The emotional aspect that comes with diabetes are also terrible. When you are low, you feel low, when you are high you feel irritable and angry. It is difficult to deal with the ups and downs. These days, the hardest part is definitely the consequences of not looking after myself in my teen years. I suffer from kidney disease, retinopathy, and neuropathy. I promise you, it’s not pleasant.
One thing you would like non diabetics to know about type 1 diabetes
It is not contagious, and we are not being punished for eating too much sugar. I cannot stress this enough. It is sad that so many people still live under this impression. Also, do not just give us sugar when we are in distress. Rather seek medical help immediately please. Also, it is not your diabetes or our diabetes, it is MY diabetes. If you see a diabetic eating a piece of cake… I am sure they injected for it, and if they didn’t, I am sure they are low or maybe just haven’t had cake in a long time. And even if it none of the above, it is not your place to scold or judge. For the most part, we know what we are doing. Just be present and be supportive, that way a diabetic will feel safe enough to confide in you when they are really in trouble. A message for newly diagnosed families Just be supportive. Do what you can to make it “nicer” and lighter. That is what Sweetner is about as well. Making things a little lighter. The little things matter and can make a world’s difference. Also, new diagnosed families can reach out to me. I am happy to chat and be supportive and give advice where I can or help you get in touch with someone who can help. Be involved in the Diabetic community. Share your worries and your successes. Try to get your kids to go to diabetic camps. I still have diabuddies that I met at camp 10 years ago. It is different connecting with someone in a similar situation. Megan Dimitriades Parents of picky eaters have increased struggles over eating, are likely to argue over the child’s eating habits, more likely to prepare a separate meal for their child, likely to offer a reward to picky eating and make comments on their children’s eating habits. Fussy Eaters eat a limited variety of food, often require food to be prepared in a specific way and have strong dislikes and likes to food. (Mascola et al 2010).
Does any of this sound familiar? Does the thought of meals stress you out and fill you with dread? Does your partner come home from work and stop and turn around at the front door as he/she cannot face the arguments that are ensuing with meal time behind the door? Fussy eating is tough on a family and then if you have the added anxiety of hypos and high blood glucose levels it becomes a battle field! YOU ARE NOT ALONE! Here are some tips for you and your family. There is not a one-size-fits-all approach as each family is different and faces different challenges.
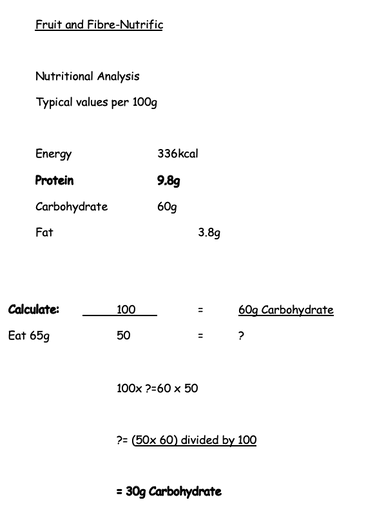
If you require additional assistance or have concerns with your child’s eating habits and nutritional status, please do not hesitate to contact me for either an online consult or face to face. You are not alone and there is help out there for feeding dilemmas. In the early days of diagnosis you might hear the term "carb counting" mentioned and have little idea of how to apply this in your journey. I recall when Harrison was diagnosed we desperately wanted to understand the principle with little guidance from our then Dr and Dietitian. Months later - possibly even a year later - we had a much better understanding of carb counting and were consequently better able to keep our little toddler Harrison in range. Now years later we are almost able to evaluate just by looking at the plate. It's often still a guessing game but to have this understanding is definitely beneficial in your type one journey. Megan has prepared an awesome blog post diving a little deeper into Carb Counting which will hopefully give you great insight that you can add to your T1D Care Toolbelt. What is Carbohydrate counting? It is working out the amount of carbohydrates in the food and drink you are having and taking the right amount of quick/rapid acting insulin to match the carbohydrates so that your blood glucose levels remain constant. Why Carbohydrate Count? So that the glucose that appears in your blood after consuming carbohydrates can be controlled by the insulin you take. The amount of carbohydrate in a food influences how much your blood glucose goes up. Each 10g carbohydrate produces about 2-3mmol of glucose in the blood. Foods contain different amounts of carbohydrate, if you know exactly how much you are eating, you will be able to work out your insulin doses more accurately. How does the insulin I take work?
New terms to learn:
What is a carbohydrate? Carbohydrate foods are often described as sugars and starches. Sugars: all foods containing added sugar (sucrose) are carbohydrate foods. They include sugar which may be added to food and
Natural sugars: the natural sugars fructose and lactose are found in fruit and milk and dairy foods and some vegetables
Starches: potato, sweet potato,· bread, rice, pasta, noodles, roti, naan bread, wraps, couscous· breakfast cereals, oats,· starchy veg - sweetcorn, peas, pumpkin, buttnernut, carrots· lentils, beans and other pulses,· all flour products e.g. pizza, pastry, baked goods, biscuits, crackers, pancakes NOTE: All carbohydrate foods produce glucose in the blood How to calculate how much carbohydrate in foods? There are many different ways of working out how much carbohydrate you are eating, you may need use a few or all of the different ways. This will depend on the types of food you have to eat. You will need to:
Sometimes you will need to weigh a food to know how big your portion size is. This will help you to know exactly how much carbohydrate you are eating. We suggest checking your portion sizes for foods like rice, pasta, noodles, baked potato, breakfast cereals. You do not need to weigh these foods every time you eat them. Make a note of your portion size in handy measures using serving spoons or measuring cups. Try and re check your portion sizes every few weeks. Tip : Use a measuring cup for foods like rice, couscous, breakfast cereal make a note in your portion book about your portion sizes. Other handy measures include:
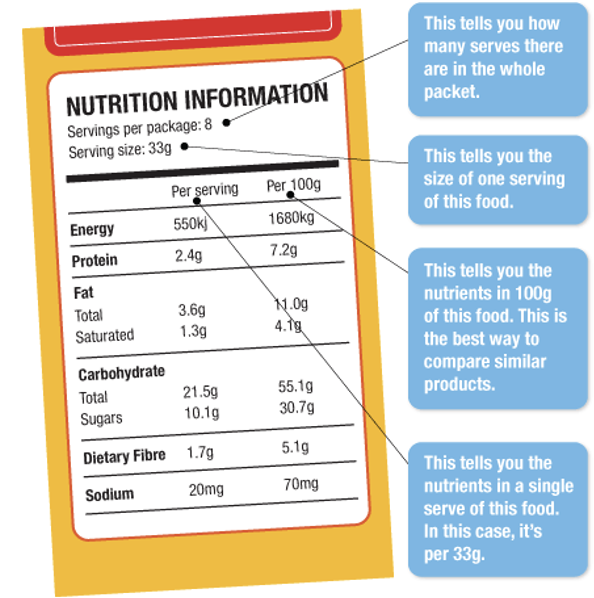
Food labels
For example a packet of dried pasta—this food label tells you about 100g of uncooked pasta But you need to know about your portion size of cooked pasta. Sometimes you may need to weigh your food and work out the amount of carbohydrate. An example may be breakfast cereals. Foods containing little or no carbohydrate
The foods below contain little or no carbohydrate, and therefore don’t really affect your blood glucose levels (when eaten in usual amounts). You still need to eat some of these foods; you just don’t “count” them when working out how much carbohydrate is in your meals.
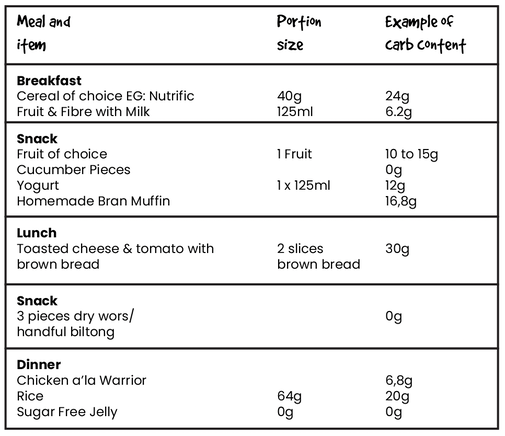
Need more help? Please get in touch via our Warrior Dietitian contact form for a 1:1 consultation Megan DimitriadesFollowing on from my previous blog post, as a dietitian, my job is to ensure that your child is eating a balanced diet that is nutritionally complete, and equipping you as the parent/caregiver with the tools to do so. Some families may prefer to have less carbs overall in their diet and this is a personal preference. There is no "one size fits all". Your child may eat more or less than this. EVERY child is different and some are more active than others, some metabolise nutrients faster or slower than others. The example below is not set out in stone but it's a guide to give you an idea of what a typical 6 year old may require on a daily basis: Potential Carb intake for an average |
| This month's feature, Bridget McNulty. Many of you might already recognise this amazing woman as one of the co-founders of the largest online Diabetes communities, Sweet Life Diabetes Community as well as of SA Diabetes Advocacy, a non-profit that brings people with Diabetes together to advocate for the rights of people living with Diabetes in South Africa. Bridget was diagnosed in 2007. She will be celebrating her 15th Diaversary next month. Below we feature our interview with her. We hope you enjoy reading this as much as we did. |
Your diagnosis story
I had just moved to Cape Town, just started my first full-time job as a Features Writer at Real Simple Magazine, and had just published my first novel called, Strange Nervous Laughter.
Life was nonstop exciting! But then I started getting insatiably hungry, and constantly thirsty, and I lost a lot of weight - no matter how much I ate. I was so exhausted that I had to take a rest after I had a shower. I eventually went to a quack of a doctor who told me I was losing weight because I ate too healthily (!) and only checked my blood sugar when I prompted him (Google is useful for some things!).
The glucometer told me my blood sugar was 25, but he sent me off into the city (on a scooter) saying I was, "practically diabetic" and had to have further blood tests. Thankfully my mom swooped into the rescue, booked me a flight home to Durban, and took me straight to ICU where I was diagnosed.
Life was nonstop exciting! But then I started getting insatiably hungry, and constantly thirsty, and I lost a lot of weight - no matter how much I ate. I was so exhausted that I had to take a rest after I had a shower. I eventually went to a quack of a doctor who told me I was losing weight because I ate too healthily (!) and only checked my blood sugar when I prompted him (Google is useful for some things!).
The glucometer told me my blood sugar was 25, but he sent me off into the city (on a scooter) saying I was, "practically diabetic" and had to have further blood tests. Thankfully my mom swooped into the rescue, booked me a flight home to Durban, and took me straight to ICU where I was diagnosed.
What do you do now for a living?
I'm the co-founder of Sweet Life Diabetes Community which is South Africa's largest online diabetes community. I'm also the co-founder and current chairperson of SA Diabetes Advocacy, a non-profit that brings all the organisations of people with diabetes together to advocate for the rights of people living with diabetes in South Africa.
My goal is to show that it's possibly for every South African with diabetes to live a happy, healthy life.
My goal is to show that it's possibly for every South African with diabetes to live a happy, healthy life.
Noteable Hypo Moments
I've only ever had two emergency diabetes moments - both within the first 3 months of having my first child. Breastfeeding has a really dramatic effect on blood sugar, and it's entirely unpredictable. Breastfeeding lows remain the most intense of my life.
When my son was 6 weeks old, I went out at night for the first time (to watch a play) and was so excited I didn't finish all my supper. My blood sugar plummeted frighteningly fast at intermission - it went from 3.5mmol/l to me not being able to speak in 5 minutes, and I passed out. An ambulance arrived quickly and I recovered very quickly but was totally spooked.
A month later, I was home in Durban for my dad's 70th and had such a fun night at his party. My blood sugar was in the 4s at bedtime, so I ate a piece of millionaire shortbread (literally sugar on sugar on sugar!) but still went dangerously low that night, and my husband had to put jam on my tongue to get me to come round. From then on I was much more careful with low blood sugar and breastfeeding, and didn't have any incidents (thankfully!) with my second child. I also think newer ultra-long-acting insulin plays a part, because it keeps your background blood sugar more stable.
When my son was 6 weeks old, I went out at night for the first time (to watch a play) and was so excited I didn't finish all my supper. My blood sugar plummeted frighteningly fast at intermission - it went from 3.5mmol/l to me not being able to speak in 5 minutes, and I passed out. An ambulance arrived quickly and I recovered very quickly but was totally spooked.
A month later, I was home in Durban for my dad's 70th and had such a fun night at his party. My blood sugar was in the 4s at bedtime, so I ate a piece of millionaire shortbread (literally sugar on sugar on sugar!) but still went dangerously low that night, and my husband had to put jam on my tongue to get me to come round. From then on I was much more careful with low blood sugar and breastfeeding, and didn't have any incidents (thankfully!) with my second child. I also think newer ultra-long-acting insulin plays a part, because it keeps your background blood sugar more stable.
What was the most difficult thing to overcome when you were first diagnosed, and how do you feel now about the same?
I thought I would never be able to eat delicious things again... I remember being devastated that I couldn't eat a piece of wedding cake at my own wedding! (I wasn't engaged or anything, just imagining the future...) Now I eat delicious things in moderation - I can live without most flavours of cake, but ice-cream is one of my favourite foods on earth, and a single scoop with a handful of nuts is fine for blood sugar!
Navigating the workplace with Type 1 Diabetes
I've never had issues with this. I have always been open about injecting and testing in the workplace, and I've been lucky to have really lovely colleagues who are supportive but mainly just leave me to my own devices!
Now that I work full-time in the diabetes space, there are plenty of us in the same boat, and we start many of our meetings saying that if anyone needs to test or inject or get a snack, they must feel free to do what they need to.
Now that I work full-time in the diabetes space, there are plenty of us in the same boat, and we start many of our meetings saying that if anyone needs to test or inject or get a snack, they must feel free to do what they need to.
Then & Now: Compare your Diabetes Regime from when you were diagnosed to now.
The biggest changes for me have been sensor technology - starting on the FreeStyle Libre felt like switching on headlights when I had been driving in the dark. And the improvements in insulin - ultra-long-acting insulin made me feel like I was standing on solid ground instead of shifting sand, and new ultra-rapid-acting insulin has given me so much flexibility back in my life.
Most annoying things people have said regarding your T1D:
It has to be, "Can you eat that?"
I just smile and say, "Yes I can!"
I just smile and say, "Yes I can!"
Your hypo symptoms:
- Racing heart
- Sweaty
- Floaty head
- Feeling jittery - the worst!
Favourite Hypo Snacks
I recently discovered Glucose C sweets from Dis-Chem and they are awesome. Softer than Super C, so easier to chew, and they act almost immediately and (crucially!) are easy to dose, without overdosing.
I start with 3 of those and then have another one or two if I need to. Also a juicebox next to my bed for night-time lows has been a game-changer (easy reaching distance, no temptation from the fridge!)
I start with 3 of those and then have another one or two if I need to. Also a juicebox next to my bed for night-time lows has been a game-changer (easy reaching distance, no temptation from the fridge!)
Positive Message for Other Type 1's
We're all in this together. It can feel so lonely, but there's a whole community of people who deeply understand what it's like to live with T1D - please join us!
Best part about being a Type 1
It forces me to do the things we should all be doing - eat well, exercise, sleep enough, look after my health - and I'm sure I'm healthier because of it.
Hardest part about being a Type 1
Never getting a holiday! Just a day off to eat ice-cream all day and not have to test would be so nice...
One thing you would like non-diabetics to know
Even if it doesn't look like it on the outside, we are doing our best. It's a constant, never-ending job, and the more supportive you can be, the better.
A message for newly diagnosed parentsEverything is going to be okay! It's so overwhelming at first, but you will fall into a rhythm and life will return to a new kind of normal. (Also! Get a free copy of our Type 1 Diabetes Guidebook - for parents here) What do you do to stay active?I walk on Chapman's Peak twice a week with a dear friend, love going on weekend hikes and nature walks, and do yoga with a very hunky online yoga instructor (Yoga with Tim). |
Your support system
My husband is wonderful - he doesn't give me too much attention about diabetes, because his brother is a Type 1 so he's used to it, but he deeply supports me in every aspect of life. My kids are very kind when I tell them I need a minute to check or correct my blood sugar. And my family and friends try to understand what it's like, but mainly just support me in every aspect of life - diabetes and otherwise.
Megan Dimitriades
The Pro's and the Con's of the most recommended diet proposed to those with Type One Diabetes. The below list of Pro's & Con's is ultimately the foundation for a much larger discussion that in time we will expand on more and more.
What do you need to know?
The Pro's
- Better blood sugar control
- It can instil a greater confidence in your own management with fewer glucose swings
- Minimises the risk of severe hypoglycaemic episodes
The Con's
- Decreased fibre intake
- Increased fat and protein intake which can lead to stress on additional organs
How low can you go?
There is no one size fits all, and different ages require different amounts of carbohydrates. Children are still growing and it is important to note that if you are cutting down on carbohydrates that you are increasing protein and fat in their diet.
Too much protein could add stress to the kidneys and more fat in their diet can increase the risk of heart disease. Cutting out carbs can also lead to vitamin deficiencies and lack of essential fibre in the diet.
There is currently a lack of evidence to state that low carb diets are fully beneficial to children. The individual child's needs to be monitored, as well as the family taken into consideration.
If you are considering low carbohydrate for your type one child, or because your child is overweight, or any other medical reason, please consult a dietitian to help you tailor make your child's diet ensuring they obtain a "nutritionally complete" diet.
Too much protein could add stress to the kidneys and more fat in their diet can increase the risk of heart disease. Cutting out carbs can also lead to vitamin deficiencies and lack of essential fibre in the diet.
There is currently a lack of evidence to state that low carb diets are fully beneficial to children. The individual child's needs to be monitored, as well as the family taken into consideration.
If you are considering low carbohydrate for your type one child, or because your child is overweight, or any other medical reason, please consult a dietitian to help you tailor make your child's diet ensuring they obtain a "nutritionally complete" diet.
How much carbs does the average child need per day?
A minimum of 130g per day, or 50 to 60% of their total energy.
The majority of carbs should come from wholegrains, vegetables, fruit and legumes.
The majority of carbs should come from wholegrains, vegetables, fruit and legumes.
Candice Christie
Nothing like the notion of Spring to give you that "fresh start" feeling. We have been quiet since COVID hit our shores and a lot in part due to the impact it had on our family at the time. This was followed by the ride of our lives as the rollercoaster of life had many unexpected things planned for us including the loss of loved ones, and the uprooting of our life in the KZN Midlands to establish new roots in good old Cape Town where we have been now for just over a year.
We haven't totally fallen off the radar and have been blessed to have made amazing friends in the Type One community here in Cape Town. Earlier this year I was invited to an event hosted by Sweet Life and Medtronic SA with a host of other "Voices for Type 1". It was such a grounding experience as a mom of a type one child to hear experiences from other parents, as well as from grown type one diabetics.
We haven't totally fallen off the radar and have been blessed to have made amazing friends in the Type One community here in Cape Town. Earlier this year I was invited to an event hosted by Sweet Life and Medtronic SA with a host of other "Voices for Type 1". It was such a grounding experience as a mom of a type one child to hear experiences from other parents, as well as from grown type one diabetics.
Behind the scenes I have made an amazing friend in Megan Dimitriades who happens to be a Dietitian that specialises in Diabetes, and especially in Paediatrics. This is in part what has spurred us on to get the ball rolling on Type One Warrior again, and to achieve our shared dreams of so many things for the type one community.
| Megan has joined the fold here at Type One Warrior and I just know she is going to bring something fresh and new to the table for us all. In the coming days we will start sharing content around some of the questions that you've been asking on our social media posts. If you hadn't been aware, you can email us on hello@typeonewarrior.co.za with content ideas or questions that you'd like addressed. We would love to hear from you! |
We have also brought back our Type One Warrior of the month feature and I am beyond excited to share the first one as we head into Spring. This first person in the new season of Type One Warrior is making the very necessary waves we need for Diabetes Awareness and has been a driving force for change in so many respects by initiating fantastic causes that bring Medical Aids up to speed with the needs of Type One families - the mindset shift of luxury items like CGM's is slowly starting to be seen as necessary for the adequate care of Type One Diabetes.
Some of you may already have guessed who will be our September Type One Warrior of the Month by the intro above. Let me leave it there though! It's going to be a goodie.
Have a blessed week further everyone... And two more days to the first day of Spring! Yay.
Some of you may already have guessed who will be our September Type One Warrior of the Month by the intro above. Let me leave it there though! It's going to be a goodie.
Have a blessed week further everyone... And two more days to the first day of Spring! Yay.
It's official. The first case of Novel Coronavirus (COVID-19) has been confirmed in South Africa - and it is on our doorstep here in our hometown, Pietermaritzburg. We certainly don't want to jump on the mania band wagon but we do feel like a little bit of preparedness towards preventing the contraction of this virus pivotal. For a Type 1 Diabetic who's immune system is already compromised this virus could wreck more havoc than we would like.
Type 1 Diabetics are at greater risk of complications when exposed to viral infections like the flu or pneumonia, and it will be no different with COVID-19. The same flu-prevention protocols are applicable: washing your hands regularly, covering coughs and sneezes with tissues, sneezing into elbow crevices, etc.
You have take advice from where it comes from and who am I to share with you anything but what I have learned from our own personal experiences? If I could offer one additional preventative measure you could implement today it would be to go out and buy any one of the Nexa Shield products and start using it.
Although I myself am not a Type 1 Diabetic, I have a preexisting condition that makes me more susceptible to respiratory infections and after three weeks of not being able to shake one, a GP recommended I start using the Nexa FluShield spray. It basically provides the nasal cavity with a powdered film lining that prevents anything from penetrating that barrier. They have several variations on the market including for allergies, kids and travelling. Ultimately they're the same product in different packaging and they work wonders.
I learned about this product on Tuesday this week and started using it straight away in sheer desperation to get rid of this cough. Within the first day I noticed my symptoms becoming clearer. At the time of the appointment with the GP he suggested taking this as a precautionary against the Coronavirus and it being suitable for someone like Harrison, our Type 1 Diabetic 4 year old son to take too.
I believe Nexa is available in most pharmacies, including Dischem. Click here to visit their website to find out more. This is not a paid post at all - just sharing because I wish I had known about this stuff sooner and I am definitely getting Harrison started on it today!
Type 1 Diabetics are at greater risk of complications when exposed to viral infections like the flu or pneumonia, and it will be no different with COVID-19. The same flu-prevention protocols are applicable: washing your hands regularly, covering coughs and sneezes with tissues, sneezing into elbow crevices, etc.
You have take advice from where it comes from and who am I to share with you anything but what I have learned from our own personal experiences? If I could offer one additional preventative measure you could implement today it would be to go out and buy any one of the Nexa Shield products and start using it.
Although I myself am not a Type 1 Diabetic, I have a preexisting condition that makes me more susceptible to respiratory infections and after three weeks of not being able to shake one, a GP recommended I start using the Nexa FluShield spray. It basically provides the nasal cavity with a powdered film lining that prevents anything from penetrating that barrier. They have several variations on the market including for allergies, kids and travelling. Ultimately they're the same product in different packaging and they work wonders.
I learned about this product on Tuesday this week and started using it straight away in sheer desperation to get rid of this cough. Within the first day I noticed my symptoms becoming clearer. At the time of the appointment with the GP he suggested taking this as a precautionary against the Coronavirus and it being suitable for someone like Harrison, our Type 1 Diabetic 4 year old son to take too.
I believe Nexa is available in most pharmacies, including Dischem. Click here to visit their website to find out more. This is not a paid post at all - just sharing because I wish I had known about this stuff sooner and I am definitely getting Harrison started on it today!
| I've been listening to podcasts for the better part of the past 3 or 4 years as a coping mechanism to help me relax and even sleep at night. I think many of you type 1 parents can probably relate - it's not always easy to fall back asleep after actively fighting lows, or highs, in the middle of the night. Pair that with mild insomnia and well - the mind just doesn't rest. I recently started listening to the juicebox podcast and was pleasantly surprised by how much I happened to be learning about things we deal with daily as parents of a Type 1 kid. They recently aired an episode called "Diabetes pro tip : Glucagon & low BGs". |
If I could recommend any episode to listen to as a starting point it would be this one! They do so well to explain, in conversational English, so much about Glucagon, when it works, when it doesn't - and then the intricacies involved in going low... boy there are many... but we knew that already didn't we? It's still worth a listen! I implore you to do so. Here's a quick link, make a cuppa tea, put your feet up and listen in.
I know I only have a 4 year old but the question of alcohol in the mix when he is older has always popped into my brain only to be brushed off by our endo when prompted: "let's worry about that when the time comes". Fair enough but having heard this podcast touch on some guidelines for people with T1D who would like to drink socially has made me feel a little less anxious knowing how to be prepared. For parents with older kids nearer the drinking age, this might be a good one for you to listen to. Aside from the drinking they speak about various other variables affecting lows, and also the efficacy of the Glucagon pen as the tool to get BG levels back up in different situations.
I know I only have a 4 year old but the question of alcohol in the mix when he is older has always popped into my brain only to be brushed off by our endo when prompted: "let's worry about that when the time comes". Fair enough but having heard this podcast touch on some guidelines for people with T1D who would like to drink socially has made me feel a little less anxious knowing how to be prepared. For parents with older kids nearer the drinking age, this might be a good one for you to listen to. Aside from the drinking they speak about various other variables affecting lows, and also the efficacy of the Glucagon pen as the tool to get BG levels back up in different situations.
| Good morning! This weekend we will be swimming the Midmar Mile for the first time as a team. Team Type One Warrior that is! We are thrilled to have rustled up a few keen swimmers and are in disbelief at the uptake of keen participants for next years swim already as well! The opportunity to represent our warriors, whether as Type 1 ourselves, or supporting someone who is, is a pleasure and a privilege because we have it on excellent authority that Type 1 Diabetics are the coolest people out and are more exceptional in many ways than most! Team pic to follow soon - for now though, here's a sneak at our team shirt. |
First things first - here's a hearty Type One Warrior "Happy New Year!" to you and your wonderful families!
We hope that 2020 is going to be a great year despite all the highs and lows that accompany life with Type One Diabetes! Sorry (not sorry) about the delay but we've been living it up in the foothills of the Drakensberg Mountains for the past week with very little cell reception!
In our family, at the start of every year we pick a word or theme to live by for the upcoming year. We've never really exercised this for our little Type One Warrior endeavours but this year we decided we should give it a bash and perhaps provide ourselves a platform that has more direction... We mulled over this for a few days and decided on a theme that might sound simple, but in actuality is all encompassing and can mean so many things.
We hope that 2020 is going to be a great year despite all the highs and lows that accompany life with Type One Diabetes! Sorry (not sorry) about the delay but we've been living it up in the foothills of the Drakensberg Mountains for the past week with very little cell reception!
In our family, at the start of every year we pick a word or theme to live by for the upcoming year. We've never really exercised this for our little Type One Warrior endeavours but this year we decided we should give it a bash and perhaps provide ourselves a platform that has more direction... We mulled over this for a few days and decided on a theme that might sound simple, but in actuality is all encompassing and can mean so many things.
Our theme for 2020 is "pursuing normalcy".
You might be sitting there thinking we've gone out of our way and over extended ourselves by choosing a goal that is far too easy and simple but if you really have a good think about it, normal can mean so many different things and needs a bit of decision making in a way - deciding what is normal for us?
Rowan and I discussed ten goals, each with their own set of micro goals that will ultimately serve as our measure in our pursuit of normalcy this year. We've listed them below.
Rowan and I discussed ten goals, each with their own set of micro goals that will ultimately serve as our measure in our pursuit of normalcy this year. We've listed them below.
Pursuing normalcy : 10 goals for 2020
Normal for us, this year, is all encompassing. We want to spend more time outdoors, we want to have tighter control over Harrison's blood glucose trends, we want to focus on creating more Type One Warrior friendly meals, we want Type One Warrior to grow as a community, we'd love to meet more Type 1 kids, and help more families affected by Type 1... there is just so much - and we want this all to be our normal!
This is in no particular order but here is our list of 10 goals we'd like to achieve this year!
Goal 1 : Improving Harrison's time-in-range and ultimately achieving an HBA1C of 6.5% or lower. Last year was all about the pump for us, and getting used to using this amazing device in the day-to-day management of Harrison's levels. For those who are not sure what a pump is, in brief, it is a small insulin-delivery device that is attached to Harrison's body and delivers the insulin that his body needs. We use it in tandem with a constant-glucose-monitor device so the full set up is like a replacement pancreas - since his no longer works. We have Harrison hooked up to the Medtronic Minimed 640G. It is an incredible system and is quite a change from having to have given 6 to 7 injections daily to now only having to change the pump site every 3 days.
Ok, back to the goal. The HBA1C is an indicator of how well you manage your Type 1 Diabetes, involving everything from what you eat, what your corresponding boluses (insulin doses) are, sick treatment, activity levels, stress levels, even the weather. We speak about time-in-range and this really refers to the healthy blood glucose level range we would like to keep Harrison in for as much time as possible. In our family this range is between 4 and 10 mmol/L.
Harrison is only 4 years old and this range will become narrower as he gets older. Because he couldn't possibly manage this all by himself, we, as his parents, are laying the foundation for a tighter control that is only going to benefit him and the decisions he makes as he grows older.
Goal 2 : Contributing more to our Type One Warrior Pantry. I seemed to achieve a lot of things during my maternity leave last year including collaborating with Fran Steart, a registered dietitian with a keen interest in Type 1 Diabetes and creating our Type One Warrior Pantry. When I headed back to work it all but fizzled out and this year we plan to get it up and running again - this time with more direction and purpose. My goal is to contribute at least 2 Type One Warrior friendly recipes a month.
Goal 3 : Getting outdoors. Along with wanting to spend more time outdoors this year, we want to become more active outdoors. So - while we would love to laze the day away in a garden chair as much as the next set of parents with two busy kids, we want to be more present with them outdoors. So more family walks and learning about nature together. In the pipeline here are lists and lists of cool outdoor activities which we will definitely be sharing because let's be honest - we could all do with a little inspiration, especially after a long week at work.
Goal 4, 5 and 6 : (4) We would like to grow Type One Warrior as a community and as a by-product hopefully (5) meet more families with Type 1 kids, and (6) be able to help more families affected by Type 1 Diabetes.
Part and parcel with goals 4, 5 and 6 is goal 7 : We would love to organise a camping trip with a few Type One Warrior families.
Goal 8 : More adventure. This year we are all about getting our camping game on again. Now that our youngest son is a year old (next week), we are feeling a bit more confident to venture out into the great unknown and experience more of the wild terrain our country has to offer. Camping is definitely going to be a norm in our family - Rowan and I were both raised loving camping and with our kids it will not differ - we hope. Our goal this year is to go on at least 6 camping trips, even if they're very local. The point is to escape from all the tech and gadgets and expose our kids to the outdoors and another way of life outside of working and living just for the weekends. We're very keen to share just how we travel and cope with Type 1 Diabetes as well - to show other Type One Warrior families that it actually is possible!
Goal 9 : Less hypos, and less treating with sweets. I suppose this could be lumped in under our first goal of tighter control over Harrison's time-in-range but I think with hypoglycaemia being the more immediately dangerous blood glucose trend requiring fast acting sugar to get his levels back up, it warrants a spot on the list. We tend to reach for sweeties as our go-to pick me up for Harrison when he is going low. Sometimes it's an available fruit or juice box, but more often than not we use wine gums or jelly babies.
Goal 10 : Type One Warrior Veggie Patch. Most of you know that we have a veggie patch at home. We have had it for the past 3 years and every year our yield improves a little more. The soil has never been 100% so we have had to make the decision now to actually work this little patch of land a little better in order for it to work better for us. We're dubbing it the Type One Warrior Veggie Patch because this is where we love spending a lot of our time as a family, and where we are trying to make a point of having much more available to Harrison to enjoy as a snack on a whim: like pulling up a carrot, or picking off some sugar snap peas or white currant tomatoes to snack on.
This is in no particular order but here is our list of 10 goals we'd like to achieve this year!
Goal 1 : Improving Harrison's time-in-range and ultimately achieving an HBA1C of 6.5% or lower. Last year was all about the pump for us, and getting used to using this amazing device in the day-to-day management of Harrison's levels. For those who are not sure what a pump is, in brief, it is a small insulin-delivery device that is attached to Harrison's body and delivers the insulin that his body needs. We use it in tandem with a constant-glucose-monitor device so the full set up is like a replacement pancreas - since his no longer works. We have Harrison hooked up to the Medtronic Minimed 640G. It is an incredible system and is quite a change from having to have given 6 to 7 injections daily to now only having to change the pump site every 3 days.
Ok, back to the goal. The HBA1C is an indicator of how well you manage your Type 1 Diabetes, involving everything from what you eat, what your corresponding boluses (insulin doses) are, sick treatment, activity levels, stress levels, even the weather. We speak about time-in-range and this really refers to the healthy blood glucose level range we would like to keep Harrison in for as much time as possible. In our family this range is between 4 and 10 mmol/L.
Harrison is only 4 years old and this range will become narrower as he gets older. Because he couldn't possibly manage this all by himself, we, as his parents, are laying the foundation for a tighter control that is only going to benefit him and the decisions he makes as he grows older.
Goal 2 : Contributing more to our Type One Warrior Pantry. I seemed to achieve a lot of things during my maternity leave last year including collaborating with Fran Steart, a registered dietitian with a keen interest in Type 1 Diabetes and creating our Type One Warrior Pantry. When I headed back to work it all but fizzled out and this year we plan to get it up and running again - this time with more direction and purpose. My goal is to contribute at least 2 Type One Warrior friendly recipes a month.
Goal 3 : Getting outdoors. Along with wanting to spend more time outdoors this year, we want to become more active outdoors. So - while we would love to laze the day away in a garden chair as much as the next set of parents with two busy kids, we want to be more present with them outdoors. So more family walks and learning about nature together. In the pipeline here are lists and lists of cool outdoor activities which we will definitely be sharing because let's be honest - we could all do with a little inspiration, especially after a long week at work.
Goal 4, 5 and 6 : (4) We would like to grow Type One Warrior as a community and as a by-product hopefully (5) meet more families with Type 1 kids, and (6) be able to help more families affected by Type 1 Diabetes.
Part and parcel with goals 4, 5 and 6 is goal 7 : We would love to organise a camping trip with a few Type One Warrior families.
Goal 8 : More adventure. This year we are all about getting our camping game on again. Now that our youngest son is a year old (next week), we are feeling a bit more confident to venture out into the great unknown and experience more of the wild terrain our country has to offer. Camping is definitely going to be a norm in our family - Rowan and I were both raised loving camping and with our kids it will not differ - we hope. Our goal this year is to go on at least 6 camping trips, even if they're very local. The point is to escape from all the tech and gadgets and expose our kids to the outdoors and another way of life outside of working and living just for the weekends. We're very keen to share just how we travel and cope with Type 1 Diabetes as well - to show other Type One Warrior families that it actually is possible!
Goal 9 : Less hypos, and less treating with sweets. I suppose this could be lumped in under our first goal of tighter control over Harrison's time-in-range but I think with hypoglycaemia being the more immediately dangerous blood glucose trend requiring fast acting sugar to get his levels back up, it warrants a spot on the list. We tend to reach for sweeties as our go-to pick me up for Harrison when he is going low. Sometimes it's an available fruit or juice box, but more often than not we use wine gums or jelly babies.
Goal 10 : Type One Warrior Veggie Patch. Most of you know that we have a veggie patch at home. We have had it for the past 3 years and every year our yield improves a little more. The soil has never been 100% so we have had to make the decision now to actually work this little patch of land a little better in order for it to work better for us. We're dubbing it the Type One Warrior Veggie Patch because this is where we love spending a lot of our time as a family, and where we are trying to make a point of having much more available to Harrison to enjoy as a snack on a whim: like pulling up a carrot, or picking off some sugar snap peas or white currant tomatoes to snack on.
Have you set some goals this year...?
Please share them with us!
We love to hear from you as well!
Towards the end of last year we featured our first Type One Warrior, Sarah Munro. We wanted this to become a regular feature, and so it will. Understandably all of our journeys are different and that, if anything, is what we are trying to illustrate! We need to read stories like this to learn that a diagnosis of type 1 diabetes is not specific to any one type of person. It crosses so many boundaries - age, race, gender, economic status. It is unpredictable to say the least.
One thing that I have noticed so far, in this journey, is that every Type One we have met is amazing! Every Type One has a story, be it a struggle or a triumph. When I first read about Marco Moolman I thought he would be a perfect fit for our next feature. Gerhard, Marco's dad, very kindly put together some highlights.
One thing that I have noticed so far, in this journey, is that every Type One we have met is amazing! Every Type One has a story, be it a struggle or a triumph. When I first read about Marco Moolman I thought he would be a perfect fit for our next feature. Gerhard, Marco's dad, very kindly put together some highlights.
Last A1C score: 7.8
Lived with T1D for: 15 years
Marco's diagnosis story
Marco was diagnosed at the age of 22 months. As a baby he was always quite a good eater but his parents very soon picked up that he had lost his appetite and became very thirsty always asking for his bottle. When his parents realised he was losing weight they took him to a GP who immediately sent them to a Pediatrician late that same night. The pediatrician listened to Marco's symptoms and tested his blood glucose (BG). It measured a shocking 40mmol! Marco was immediately admitted into ICU and his parents were told that their baby boy was a Type One Diabetic.
"At that stage we had no frame of reference as our daughter, 3 years older than Marco, had nothing of the sort. Nor did anyone else in the family. We felt totally lost and overwhelmed with all the information and advice from the Doctor and nursing staff. Who do we listen to? Where do we turn to at night when BG levels just won't settle? We sometimes felt as if we were in a dark hole with nowhere to run. Reality is, we later realised, there is nowhere to run. You have to, simply put, face what is thrown your way. Everyday without fail!", Gerhard shared.
Hypoglycaemic moments
Marco has had four setbacks where he went into a hypoglycaemic coma because of dangerously low BG levels. On these days, Gerhard recalls him and his wife feeling like total failures. As time moved on they realised that they could only ever do their best, no more, no less.
Going to school
Sending Marco to preschool was a huge challenge. The Moolman's were faced with having to place their responsibility of caring for their child into the hands of others. Marco was 4 when he started preschool and Gerhard recalls the challenge of feeling like their child was their responsibility and not that of caregivers. Sending him off to primary school was an even greater challenge.
"Even though, as a parent, you want to wrap your Diabetic child up in cotton wool and protect him from whatever the world throws at them, we decided to expose Marco to as much normal as possible!"
Lived with T1D for: 15 years
Marco's diagnosis story
Marco was diagnosed at the age of 22 months. As a baby he was always quite a good eater but his parents very soon picked up that he had lost his appetite and became very thirsty always asking for his bottle. When his parents realised he was losing weight they took him to a GP who immediately sent them to a Pediatrician late that same night. The pediatrician listened to Marco's symptoms and tested his blood glucose (BG). It measured a shocking 40mmol! Marco was immediately admitted into ICU and his parents were told that their baby boy was a Type One Diabetic.
"At that stage we had no frame of reference as our daughter, 3 years older than Marco, had nothing of the sort. Nor did anyone else in the family. We felt totally lost and overwhelmed with all the information and advice from the Doctor and nursing staff. Who do we listen to? Where do we turn to at night when BG levels just won't settle? We sometimes felt as if we were in a dark hole with nowhere to run. Reality is, we later realised, there is nowhere to run. You have to, simply put, face what is thrown your way. Everyday without fail!", Gerhard shared.
Hypoglycaemic moments
Marco has had four setbacks where he went into a hypoglycaemic coma because of dangerously low BG levels. On these days, Gerhard recalls him and his wife feeling like total failures. As time moved on they realised that they could only ever do their best, no more, no less.
Going to school
Sending Marco to preschool was a huge challenge. The Moolman's were faced with having to place their responsibility of caring for their child into the hands of others. Marco was 4 when he started preschool and Gerhard recalls the challenge of feeling like their child was their responsibility and not that of caregivers. Sending him off to primary school was an even greater challenge.
"Even though, as a parent, you want to wrap your Diabetic child up in cotton wool and protect him from whatever the world throws at them, we decided to expose Marco to as much normal as possible!"
Marco's journey
At the age of four, Marco started on the pump. This made a huge difference in his Diabetes Management. He was very sporty from a young age and played rugby, hockey and started cycling at the age of 9.
School tours and camps were always challenging but Marco's parents managed to send him on every camp. Either mom or dad joined the camp, staying in a nearby guesthouse or hiding between teachers.
When Marco started highschool he decided to concentrate on his hockey and cycling. He played in the A side for his school every year and formed part of the school's mountain bike team that has won the Spur Highschool MTB National Series for 3 years running. Marco was the only Type One Diabetic cyclist at the Nationals and finished int he Top 10 in his age category every year.
At the age of four, Marco started on the pump. This made a huge difference in his Diabetes Management. He was very sporty from a young age and played rugby, hockey and started cycling at the age of 9.
School tours and camps were always challenging but Marco's parents managed to send him on every camp. Either mom or dad joined the camp, staying in a nearby guesthouse or hiding between teachers.
When Marco started highschool he decided to concentrate on his hockey and cycling. He played in the A side for his school every year and formed part of the school's mountain bike team that has won the Spur Highschool MTB National Series for 3 years running. Marco was the only Type One Diabetic cyclist at the Nationals and finished int he Top 10 in his age category every year.
"In 2016 we were made aware of Team Novo Nordisk, a pro cycling team in the USA that consisted of only Type One Diabetic cyclists. Marco was invited to join their Talent ID Camp at the Georgia University in Athens, Georgia in 2017. He was the first South African cyclist to be invited and really made a big impression in the USA."
Roll on February 2018, and we were informed that Marco had made the Junior Team of cyclists from around the globe to race in Belgium, Canada and USA under the banner of Team Type 1 Foundation, a feeding team for Team Novo Nordisk Pro Cycling. He will be travelling abroad in April and July of this year for Junior Tours against the top Junior cyclists the world has to offer. This racing can be described as one level below Junior World Champs.
Marco has just returned from Belgium and Holland where he played several hockey tournaments. He was one of two Type 1 Diabetics from his school that went on tour and everything went well. Marco managed his BG levels well and has no issues. Naturally he hated the Diabetic diet someone ordered for him on his flight - that being the worst part of the tour.
He's back in Belgium from 25 April until 22 May competing in the World Class Junior Cycling Tours and Races. There are 8 to 10 races that he will be competing in as part of the Type 1 Foundation Junior Cycling Team. Only 8 Type 1 cyclists from around the world are selected, Marco being the first South African ever.
Roll on February 2018, and we were informed that Marco had made the Junior Team of cyclists from around the globe to race in Belgium, Canada and USA under the banner of Team Type 1 Foundation, a feeding team for Team Novo Nordisk Pro Cycling. He will be travelling abroad in April and July of this year for Junior Tours against the top Junior cyclists the world has to offer. This racing can be described as one level below Junior World Champs.
Marco has just returned from Belgium and Holland where he played several hockey tournaments. He was one of two Type 1 Diabetics from his school that went on tour and everything went well. Marco managed his BG levels well and has no issues. Naturally he hated the Diabetic diet someone ordered for him on his flight - that being the worst part of the tour.
He's back in Belgium from 25 April until 22 May competing in the World Class Junior Cycling Tours and Races. There are 8 to 10 races that he will be competing in as part of the Type 1 Foundation Junior Cycling Team. Only 8 Type 1 cyclists from around the world are selected, Marco being the first South African ever.
One difficult thing Marco has had to overcome being Type 1 Diabetic: Having to eat selectively, and not whatever he wants when he wants.
Favourite hypo snack: Doritos - the blue packet!
Positive message for other Type One Warriors: Life with T1D just needs more discipline. You are able to do ANYTHING you want and don't have to stand back for anyone or anything! Take life by the horns and make a difference. Diabetes is not something you chose, Diabetes chose you.
Best part about being a Type 1: Being able to have snacks during class when your BG levels are low.
One thing Marco would love non-diabetics to know about Type 1 Diabetes: Type 1 Diabetes is not caused by eating sweets. People threaten their kids with Diabetes when they eat sweets and that is VERY wrong. T1D is also not transferable.
For newly diagnosed families, Marco has this to say:
"I have been living with Diabetes basically my whole life, from the age of 22 months, so you're going to be fine. Don't let life get you down and live like the warrior you were chosen to be. To the parents I would like to say, take it day by day. Your child has a full life ahead of him/her. Nothing you did wrong caused Diabetes, so team up and manage it."
You can follow Marco on his instagram here!
Favourite hypo snack: Doritos - the blue packet!
Positive message for other Type One Warriors: Life with T1D just needs more discipline. You are able to do ANYTHING you want and don't have to stand back for anyone or anything! Take life by the horns and make a difference. Diabetes is not something you chose, Diabetes chose you.
Best part about being a Type 1: Being able to have snacks during class when your BG levels are low.
One thing Marco would love non-diabetics to know about Type 1 Diabetes: Type 1 Diabetes is not caused by eating sweets. People threaten their kids with Diabetes when they eat sweets and that is VERY wrong. T1D is also not transferable.
For newly diagnosed families, Marco has this to say:
"I have been living with Diabetes basically my whole life, from the age of 22 months, so you're going to be fine. Don't let life get you down and live like the warrior you were chosen to be. To the parents I would like to say, take it day by day. Your child has a full life ahead of him/her. Nothing you did wrong caused Diabetes, so team up and manage it."
You can follow Marco on his instagram here!
Everyone knows that when a T1D is sick, their sugar levels are affected hugely. Either you're fighting ridiculous lows, or the total inverse, sky-high hypers that are tough as nails to get down! So this flu Harrison has caught has us fighting more highs than lows and a new problem that we're facing compared, to other sensors we've inserted, are false readings on Harrison's CGM.
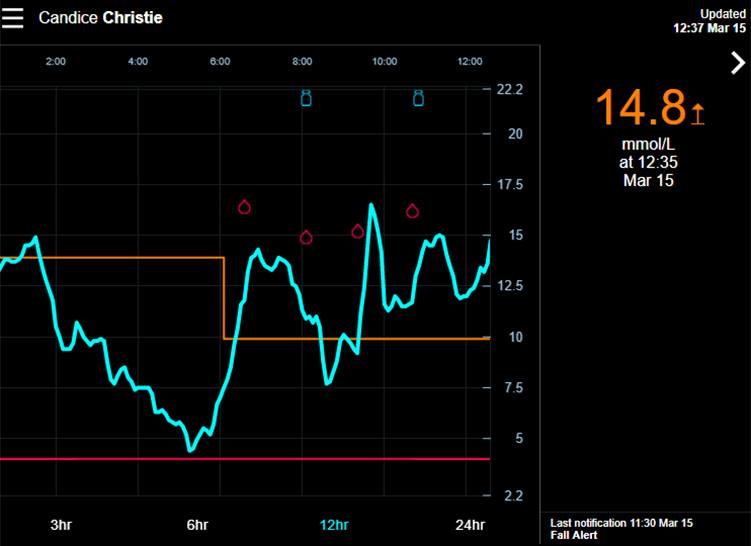
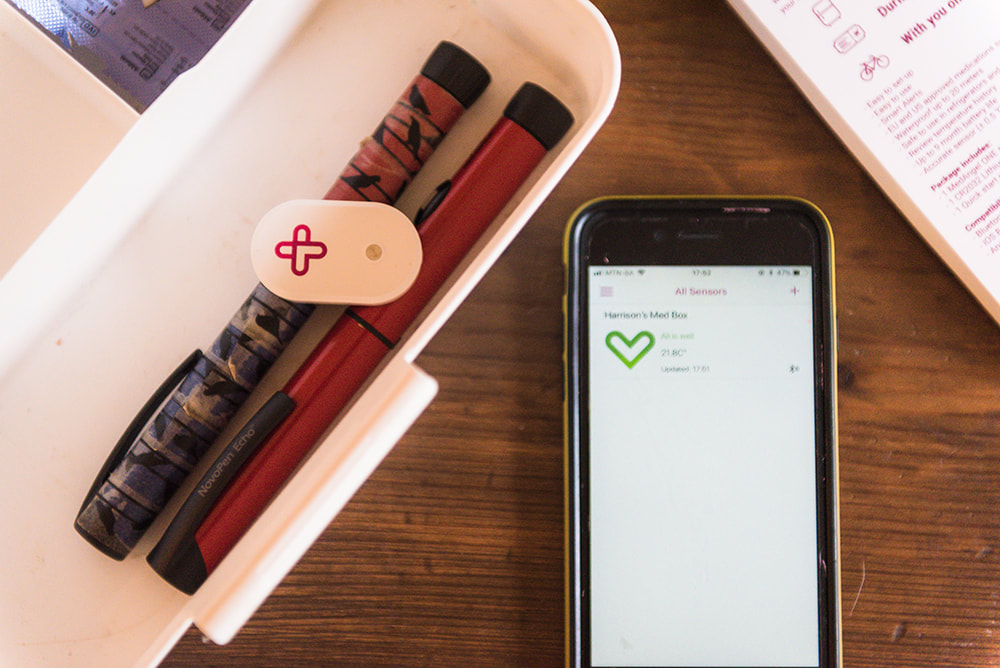
A CGM is a device that is attached to Harrison. There is a little filament embedded in the interstitial fluid under the skin that gives us a "constant glucose reading". Harrison has the Medtronic Gaurdian Connect. These little sensors don't last forever. We insert a new one every 6 days. These devices cost a premium and they are not 100% accurate all the time. The boxes all come with a warning that you're not to treat based on sensor readings output by the CGM - that you need to perform a blood glucose test to make a treatment decision.
If you look at the graph above you'll note all the little blood drops. These blood drops indicate blood tests that we have physically done and then input into the sensor for calibration purposes. The blue line is what the sensor reading is. Every single time a coconut the variance between what the blood test result is, and what the sensor is saying, is vastly different. He was running much higher than what the sensor was saying.
I shared this on our social media platforms, Instagram and Facebook and a very awesome lady, Vivian Lee Levin, shared an article with me that some medications seem to have this effect on sensor readings. Here's the article! Might I add we were hours away from possibly removing the sensor, even though it had only been inserted two days prior. We were convinced we had a dud but then Vivian shared this article with me.
We haven't changed anything from the usual medication we give him when fluey, but I decided to have a look at some of the ingredients in the meds to see if it might be a possibility. So if you read the article mentioned above, they indicate that "acetaminophen can falsely elevate sensor glucose readings". In our case the inverse is happening but the fact remains that medication affects sensor reading and as I have learned with Harrison, he often has the opposite to the adverse effects of meds. For example, Allergex is meant to make people drowsy - not Harrison. He get's restless and hyperactive.
So, we've been giving him Corenza C syrup for kids. It is sugar free but contains paracetamol, a p-aminophenol derivative. Making it part of the family of drugs that seems to affect sugar levels. Paracetamol is in A LOT of medication.
I have to note that we've used Corenza C often for flu but it has never had this effect before. But maybe there are environments (his body) that are sometimes more sensitive than others to these sorts of effects.
The below excerpt from the article sums the effect up nicely:
If you look at the graph above you'll note all the little blood drops. These blood drops indicate blood tests that we have physically done and then input into the sensor for calibration purposes. The blue line is what the sensor reading is. Every single time a coconut the variance between what the blood test result is, and what the sensor is saying, is vastly different. He was running much higher than what the sensor was saying.
I shared this on our social media platforms, Instagram and Facebook and a very awesome lady, Vivian Lee Levin, shared an article with me that some medications seem to have this effect on sensor readings. Here's the article! Might I add we were hours away from possibly removing the sensor, even though it had only been inserted two days prior. We were convinced we had a dud but then Vivian shared this article with me.
We haven't changed anything from the usual medication we give him when fluey, but I decided to have a look at some of the ingredients in the meds to see if it might be a possibility. So if you read the article mentioned above, they indicate that "acetaminophen can falsely elevate sensor glucose readings". In our case the inverse is happening but the fact remains that medication affects sensor reading and as I have learned with Harrison, he often has the opposite to the adverse effects of meds. For example, Allergex is meant to make people drowsy - not Harrison. He get's restless and hyperactive.
So, we've been giving him Corenza C syrup for kids. It is sugar free but contains paracetamol, a p-aminophenol derivative. Making it part of the family of drugs that seems to affect sugar levels. Paracetamol is in A LOT of medication.
I have to note that we've used Corenza C often for flu but it has never had this effect before. But maybe there are environments (his body) that are sometimes more sensitive than others to these sorts of effects.
The below excerpt from the article sums the effect up nicely:
"It's very important that the effect of acetaminophen on CGM — and its magnitude — be known, especially as CGM technology is being used increasingly by patients. Also, with artificial-pancreas technology rapidly advancing and with the potential for insulin dosing based on CGM instead of only with meter glucose, this is an important topic," Dr Maahs told Medscape Medical News.
The 40 subjects had a mean age 28.5 years and HbA1c 7.3%. They all used the Dexcom system.
After taking 1000 mg of acetaminophen, the subjects performed finger-stick blood glucose checks at 30 minutes and 1, 2, 4, 6, and 8 hours. There were significant differences between the CGM and meter readings (P < .01) for the entire 8-hour period. The greatest mean difference was 61 mg/dL, occurring at 2 hours, but there was a wide range of individual variation.
The phenomenon would be expected to affect the CGM's reporting of blood glucose trends as well as individual readings. "The impact of acetaminophen is greatest at approximately 2 hours, with a diminishing effect over 8 hours, so acetaminophen could have an effect on glycemic trends as its effect peaks and wanes," Dr Maahs told Medscape Medical News.
Newer technology is being developed to further limit or eliminate this effect. "Until those technologies are available, this is an important issue for patients and clinicians to be aware of," he said, adding, "This should not discourage CGM use but rather inform and educate people. In fact, our study group is an advocate of CGM use for people with type 1 diabetes."
We're only 16 months in, but it feels like a lifetime of Type 1 Diabetes already! If you come to think of it, Harrison has lived with Type 1 Diabetes longer than he has lived without it. Diagnosed at 11 months old, we have navigated many frustrations with brave faces and worried hearts - from fussy eating after bolusing (injecting for meals to cover the impending blood sugar spike), to our first hypoglycaemic seizure (from his blood sugars dropping too low), to teething sugar spikes, to fighting tummy bugs in hospital on glucose drips!
Often normal toddler ailments, like fussy eating and teething, even a little tummy bug, are shrugged off by parents of non-diabetic children as normal, but as I am sure most Type 1 parents would agree - throw small things like these in the mix of already unpredictable sugar levels and you're set for amplified nights of no sleep, extra bolusing, extra finger pricks, extra midnight snacking - the works! The game is never over, there is never a winner, it's all about balance.
I often get asked in passing "How's Harrison?", "How are you guys coping?" - these are easy enough to answer although I often feel my answer is always the same because in passing you can't really get down to the nitty gritty of how it all is actually going! I give everyone the benefit of the doubt, that they really want to know - the truth of the matter is that Type 1 Diabetes is our new normal so for me to say it's all going well, I do in fact mean it is. It's hard, but it's our life now, we have no choice. Suck it up and LIVE!
From the outside looking in, a normal day in our life involves a host of life-saving decisions and actions that parents of children without Type 1 Diabetes might not necessarily have to worry about. These aren't really questions that can be answered in passing so the short and sweet of it is that we are making it work and we are surviving.
Since Harrison was born we have never reflected on our lives as much as we do now, and especially so after Harrison was diagnosed. Paired with life events of losing friends long before their time we have realised that our lives are meant to be lived! We have made some promises to ourselves and one of them is every chance we get we are going camping. We love camping and always dreamed we would bring our children up with the same love for the outdoors and for camping. Diabetes MUST NOT change dreams like these and I think all too often it does for some.
I am not one of those people who happens to be extra positive and happy 24/7. Every glass in the world shattered for us when we heard the words "Your son is Type 1 Diabetic" and for a long time after we heard them we struggled to process this news. We cried. A lot. We blamed ourselves. We blamed others. We sat in silence a lot. We hugged Harrison every chance we got. We gave him plenty of kisses. We basically smothered him! Grief overcame us but at some point we had to force ourselves to find something positive! We took so much solace from the fact that our son fought with all his might and the entire time that he fought he wore his cheerful smile. He was weak, couldn't walk, barely babbled, but he smiled for us all the time!
Life has to carry on! You're going to adapt. It is going to carry on! It will be different. It will be harder. But you will be able to do it!
I have had some friends remark that they could never give their child an injection... perhaps one or two of you feel the same. I can assure you that when faced with a lifetime of injections or the possibility of a life without your child you will man up and step up to the plate! In the beginning they're uncomfortable but after a few weeks they go unnoticed. We opted for 4mm needles on our penfills for Harrison and before ever giving him his first injections ourselves we injected each other to feel what he would feel - in truth we barely felt it.
In the beginning you are bombarded with so much information. Every minute spent in hospital is torture because this world you have been thrown into is so foreign. You're continually being fed information, and then tested on what you learn. Emotionally there is absolutely nobody there for you but yourselves. There's a psychologist in the mix of doctors who oversee you but they are only their to check your mental state before giving the "OK" for you to leave the hospital and deal with this on your own. Emotionally there is a big fat void.
You need to find strength and courage from a place you don't know that you have! 16 months in and sometimes the same applies! With these recollections of the "early days", my strongest recommendation to new T1D families would be to sign up to the community of parents who have been through what you are going through. Type One Warrior is one such place - we encourage you to reach out to us via Facebook messenger or even email. We are preparing a Type One Warrior lifeline and information pack that will help you through these early days. Pop us an email and let us know what you're going through! There is also a fantastic Facebook group called "Kids Powered by Insulin" that is filled with parents ready to impart their words of encouragement when your child is first diagnosed!
Often normal toddler ailments, like fussy eating and teething, even a little tummy bug, are shrugged off by parents of non-diabetic children as normal, but as I am sure most Type 1 parents would agree - throw small things like these in the mix of already unpredictable sugar levels and you're set for amplified nights of no sleep, extra bolusing, extra finger pricks, extra midnight snacking - the works! The game is never over, there is never a winner, it's all about balance.
I often get asked in passing "How's Harrison?", "How are you guys coping?" - these are easy enough to answer although I often feel my answer is always the same because in passing you can't really get down to the nitty gritty of how it all is actually going! I give everyone the benefit of the doubt, that they really want to know - the truth of the matter is that Type 1 Diabetes is our new normal so for me to say it's all going well, I do in fact mean it is. It's hard, but it's our life now, we have no choice. Suck it up and LIVE!
From the outside looking in, a normal day in our life involves a host of life-saving decisions and actions that parents of children without Type 1 Diabetes might not necessarily have to worry about. These aren't really questions that can be answered in passing so the short and sweet of it is that we are making it work and we are surviving.
Since Harrison was born we have never reflected on our lives as much as we do now, and especially so after Harrison was diagnosed. Paired with life events of losing friends long before their time we have realised that our lives are meant to be lived! We have made some promises to ourselves and one of them is every chance we get we are going camping. We love camping and always dreamed we would bring our children up with the same love for the outdoors and for camping. Diabetes MUST NOT change dreams like these and I think all too often it does for some.
I am not one of those people who happens to be extra positive and happy 24/7. Every glass in the world shattered for us when we heard the words "Your son is Type 1 Diabetic" and for a long time after we heard them we struggled to process this news. We cried. A lot. We blamed ourselves. We blamed others. We sat in silence a lot. We hugged Harrison every chance we got. We gave him plenty of kisses. We basically smothered him! Grief overcame us but at some point we had to force ourselves to find something positive! We took so much solace from the fact that our son fought with all his might and the entire time that he fought he wore his cheerful smile. He was weak, couldn't walk, barely babbled, but he smiled for us all the time!
Life has to carry on! You're going to adapt. It is going to carry on! It will be different. It will be harder. But you will be able to do it!
I have had some friends remark that they could never give their child an injection... perhaps one or two of you feel the same. I can assure you that when faced with a lifetime of injections or the possibility of a life without your child you will man up and step up to the plate! In the beginning they're uncomfortable but after a few weeks they go unnoticed. We opted for 4mm needles on our penfills for Harrison and before ever giving him his first injections ourselves we injected each other to feel what he would feel - in truth we barely felt it.
In the beginning you are bombarded with so much information. Every minute spent in hospital is torture because this world you have been thrown into is so foreign. You're continually being fed information, and then tested on what you learn. Emotionally there is absolutely nobody there for you but yourselves. There's a psychologist in the mix of doctors who oversee you but they are only their to check your mental state before giving the "OK" for you to leave the hospital and deal with this on your own. Emotionally there is a big fat void.
You need to find strength and courage from a place you don't know that you have! 16 months in and sometimes the same applies! With these recollections of the "early days", my strongest recommendation to new T1D families would be to sign up to the community of parents who have been through what you are going through. Type One Warrior is one such place - we encourage you to reach out to us via Facebook messenger or even email. We are preparing a Type One Warrior lifeline and information pack that will help you through these early days. Pop us an email and let us know what you're going through! There is also a fantastic Facebook group called "Kids Powered by Insulin" that is filled with parents ready to impart their words of encouragement when your child is first diagnosed!
Towards the end of last year I stumbled across an Instagram post about the MedAngel ONE Insulin Temperature Sensor. I very quickly got in touch with the Germany-based company and was blown away by how quickly my email was received and replied to. Our new temperature sensors arrived this week, and as luck would have it - it has been the hottest week in months. We experienced first hand the little sensor readings being received by the app on our phone and then alarming to alert us to the temperature rise. We quickly moved our insulin into the fridge for it to cool down for the remainder of the afternoon before needing it again at Harrison's dinnertime bolus and bedtime basal.
I think we waited about 4 or 5 weeks for our sensors to arrive, and you can imagine that when it did, we very eagerly ripped open the envelope and sensor box to get going. We then spent about 5 minutes navigating the super easy app... and then spent the rest of the night checking the insulin temperature every few minutes! It felt like the first few hours after a CGM insertion. Of course the novelty wears off because the temperature doesn't fluctuate abnormally in the evenings for us to be aware or take precautions in a hurry.
This past week we have had some incredibly high temperatures and the app has been able to notify us several times of an increase that we were then able to move our insulin into a fridge. Had we not had these in place we'd have lost his basal and bolus cartridges to the spoils of Summer.
Here's our unboxing in pics:
This past week we have had some incredibly high temperatures and the app has been able to notify us several times of an increase that we were then able to move our insulin into a fridge. Had we not had these in place we'd have lost his basal and bolus cartridges to the spoils of Summer.
Here's our unboxing in pics:
In a couple weeks we will share some more about this nifty little gadget. Aside from proving itself useful in this heat, we were thrilled to see that it can store temperature data for up to 7 days in the absence of the app. How cool?
MedAngel Co is offering FREE SHIPPING when you use our coupon code: TYPEONEWARRIOR
Click through to place your order here. And don't forget to use TYPEONEWARRIOR at checkout so that you get free shipping - Thanks MedAngel Co for being so awesome to us South Africans who very rarely benefit from worldwide tech advances first with the rest of the world, especially with regards to beneficial Diabetes related care.
MedAngel Co is offering FREE SHIPPING when you use our coupon code: TYPEONEWARRIOR
Click through to place your order here. And don't forget to use TYPEONEWARRIOR at checkout so that you get free shipping - Thanks MedAngel Co for being so awesome to us South Africans who very rarely benefit from worldwide tech advances first with the rest of the world, especially with regards to beneficial Diabetes related care.
Below is a link shared on our insta showing how the cool little app alerted us to the temp going too high! If you don't follow us on instagram yet, make sure that you do! We are @typeonewarrior.co.za - or simply click through here and you can hit follow on our profile!
A post shared by type one warrior (@typeonewarrior.co.za) on
Before we head off on our big road trip to Port Elizabeth with our toddler and our Keto pup, we thought we would share a quick update and maybe give a bit more insight into Keto's training and what it will mean for us having a Diabetic Alert Dog when he starts alerting to Harrison's highs and lows. Posts about Keto's training can be found under D.A.D. 101 - the abbreviation DAD obviously means Diabetic Alert Dog.
What is a Diabetic Alert Dog (DAD)?
Simply put, a DAD is a dog that has been trained to alert for scent changes in the saliva of a Diabetic that are markers for a high or low blood glucose level. How he will alert depends on what we train him to do when he picks up on these scents. We are considering a high alert to be a nudge with his nose on our person, and a low to be a physical raising of the paw and prodding us with it - like a "hey you" prod.
In the context of our home, and the relationship that we have with dogs, Keto is going to be filling several roles. He is a companion for Harrison first and foremost. We are investing hugely into positively reinforcing good interaction between both Keto and Harrison. It's funny... Right now I am reading two books consecutively: Training your Diabetic Alert Dog by Rita Martinez & Susan M Barns, as well as New Toddler Taming by Dr Christopher Green. How apt that this is all happening at the same time! Training a Diabetic Alert Dog and Taming a Toddler! We believe there is a lot of value in the bond between doggie and kiddie and a lot can be learned from these relationships.
Simply put, a DAD is a dog that has been trained to alert for scent changes in the saliva of a Diabetic that are markers for a high or low blood glucose level. How he will alert depends on what we train him to do when he picks up on these scents. We are considering a high alert to be a nudge with his nose on our person, and a low to be a physical raising of the paw and prodding us with it - like a "hey you" prod.
In the context of our home, and the relationship that we have with dogs, Keto is going to be filling several roles. He is a companion for Harrison first and foremost. We are investing hugely into positively reinforcing good interaction between both Keto and Harrison. It's funny... Right now I am reading two books consecutively: Training your Diabetic Alert Dog by Rita Martinez & Susan M Barns, as well as New Toddler Taming by Dr Christopher Green. How apt that this is all happening at the same time! Training a Diabetic Alert Dog and Taming a Toddler! We believe there is a lot of value in the bond between doggie and kiddie and a lot can be learned from these relationships.
Why would we want a DAD for Harrison?
It goes without saying that whilst technology is so advanced there are still downfalls particularly with regards to an affordable Constant Glucose Monitoring (CGM) device that is 100% accurate, 100% of the time. That is unheard of. Harrison is also very young still (now 2 years old) and not yet fully able to let us know when he starts feeling a "high" or "low" glucose level coming on. CGM's are also not usually quick enough to alert in time to take action to curb the high or low without feeling the pressure of rushed treating.
Having a DAD will mean we have tighter control over these fluctuations in glucose levels which will inevitably promote a healthy and long life with fewer negative implications of Diabetes over a long period of time.
Without having to go into too much detail, the crux is that a well trained DAD will alert to a rapid fluctuation well before the CGM picks up the downward or upward trend. Time is of the essence in glucose control, especially in the "low glucose" realm. Hypoglycaemia can put patients at immediate risk of seizures and even comas. If not treated in time by quickly giving a dose of sugar, or in more dangerous situations the Glucagon pen, it may not end well. With a dog alerting to the trend, a patient can quickly test and administer the necessary glucose to curb it dropping out of the safe zone.
It goes without saying that whilst technology is so advanced there are still downfalls particularly with regards to an affordable Constant Glucose Monitoring (CGM) device that is 100% accurate, 100% of the time. That is unheard of. Harrison is also very young still (now 2 years old) and not yet fully able to let us know when he starts feeling a "high" or "low" glucose level coming on. CGM's are also not usually quick enough to alert in time to take action to curb the high or low without feeling the pressure of rushed treating.
Having a DAD will mean we have tighter control over these fluctuations in glucose levels which will inevitably promote a healthy and long life with fewer negative implications of Diabetes over a long period of time.
Without having to go into too much detail, the crux is that a well trained DAD will alert to a rapid fluctuation well before the CGM picks up the downward or upward trend. Time is of the essence in glucose control, especially in the "low glucose" realm. Hypoglycaemia can put patients at immediate risk of seizures and even comas. If not treated in time by quickly giving a dose of sugar, or in more dangerous situations the Glucagon pen, it may not end well. With a dog alerting to the trend, a patient can quickly test and administer the necessary glucose to curb it dropping out of the safe zone.
What we have accomplished so far?
Keto is 17 weeks old and has recently graduated from Puppy Classes with Adrienne's Puppy School based here in Pietermaritzburg, KwaZulu-Natal where we live. He was a star pupil and has an exciting little future ahead of him. He has been enrolled in obedience classes for next year and over the next few weeks we will be introducing a clicker into his training which will make the reinforcement of correct behavior easier especially as we start exposing him to new environments and of course, scent training and alerting for these scents.
Where we are heading?
As mentioned above we are going to commence scent training in the next few weeks with Keto. Things likely happen a lot slower in our home as we are training him ourselves with regards to the Diabetic Alerting at the same time as raising a toddler and of course working full time. Every morsel of time is essential so when there is a moment free we are trying our darnedest to get this right.
Keto is 17 weeks old and has recently graduated from Puppy Classes with Adrienne's Puppy School based here in Pietermaritzburg, KwaZulu-Natal where we live. He was a star pupil and has an exciting little future ahead of him. He has been enrolled in obedience classes for next year and over the next few weeks we will be introducing a clicker into his training which will make the reinforcement of correct behavior easier especially as we start exposing him to new environments and of course, scent training and alerting for these scents.
Where we are heading?
As mentioned above we are going to commence scent training in the next few weeks with Keto. Things likely happen a lot slower in our home as we are training him ourselves with regards to the Diabetic Alerting at the same time as raising a toddler and of course working full time. Every morsel of time is essential so when there is a moment free we are trying our darnedest to get this right.
I am hopeful that this will become a regular feature on our Type One Warrior page. A warrior feature that proves, above all else, that type one diabetes does not discriminate. It affects all races, all ages, all genders and all socio-economic backgrounds. The more stories we read the more we learn about the disease and how different every single person’s journey is.
Sarah Munro is a 27-year old mom. She was one of the first friends who came to our side when Harrison was diagnosed over a year ago. Sarah has been fighting Type 1 Diabetes along with a few subsequent ailments for 17 years.
Sarah Munro is a 27-year old mom. She was one of the first friends who came to our side when Harrison was diagnosed over a year ago. Sarah has been fighting Type 1 Diabetes along with a few subsequent ailments for 17 years.
Last A1C score: 6.8
Lived with T1D for: 17 years
My diagnosis story
I was really sick. The previous year I had been diagnosed with bronchitis and from there I had started losing a lot of weight. I was 10 years old and looked like a rake. I remember going to see a friend of mine's gran in hospital one day and the lady lying next to her had diabetes. I didn't know anything about diabetes at the time but my friend told me that she was dying. Around the same time, my mom got really worried about my weight loss and took me to the doctor. He sent me off for blood tests and we went home.
I'll never forget that phone call at home: I answered the phone and it was the doctor. He asked to speak to my mom. We had another phone in my parents bedroom and she went there to talk to him. She started crying, and when she got off the phone she came and told me that I had diabetes and I needed to get to hospital.
I remember thinking about that elderly lady lying in hospital and I just started crying saying 'I don't want to die'. My blood glucose level was at 39, a non diabetic's ideal blood glucose level ranges from 4-6mmol/L.
I have a huge needle phobia so learning to inject myself and check my own sugars was a huge battle for me.
Dealing with Type 1 Diabetes in public as a child and teen
I have never necessarily been ashamed of being a Type 1 Diabetic, I’ve just never advertised it. When I was diagnosed the teacher at my school educated the class about diabetes. The friends I had were really supportive and most of these friends ended up attending the same high school as me so that adjustment was easy.
I met a friend on one of the diabetic camps and he would openly inject himself at the dinner table even through his jeans. I preferred to go away from people (usually the bathroom) to inject myself, but that was more because I was so afraid of people bumping me while I was injecting.
The most difficult thing to overcome being diagnosed a Type 1 Diabetic
Shew! I have found each phase of life has had such a different battle. Initially learning how to inject was tough. In hospital they taught me with a needle and an orange. Going back to school was also tough as I had missed a lot and trying to catch up was very stressful.
The pre-teen years were tough as we were still in the learning phase and adjusting medication. During my time of facing how to inject myself despite my fear, I went through what is known as the "honeymoon period'. This is when your pancreas kicks in a little and gives its last couple of squirts of insulin. Because my body was producing small amounts of insulin, the amount of insulin needed via injection was greatly reduced. I was starting to have hypos (episode of hypoglycaemia where your body has too little glucose going to the brain) but the doctor encouraged my mom to continue trying to get me used to injecting even if it was half a unit, or none at all.
My teen years were terrible. Hormones caused many issues for my sugars, often ending me up in DKA in hospital, and twice in a coma. With the added stress of exams and what to study or where to study - it was all just such a mess. Varsity was another challenge: the extra independence came with extra responsibility. Going out for drinks with friends wasn't as simple as just choosing what drink to have or whose house to have pre-drinks at. Clubbing, cocktails, shooters lead to late night/early morning burgers or feasts at the local clubs hotdog stand.
The next challenge was when I was pregnant. I had a terrible pregnancy. I was diagnosed with pre-eclampsia at 12 weeks and soon after I was diagnosed with hyper-emesis gravadium. My kidneys very quickly started showing signs of deterioration and I was battling terribly with my eyesight. My HbA1c was the best it has ever been in a long time when I was pregnant because of how disciplined I was - I had a strong motivation to be healthy. My baby was born at 26 weeks and this is the only time I have ever been grateful for my Diabetes. Diabetic women are known to have larger babies due to the excess sugar which in turn, makes the baby secrete extra insulin which then increases the fat deposits in the baby. My baby boy was only 300gms over the usual weight of a 26 week gestation baby, but any NICU mom will tell you that 300gms is a LOT!
To date, the most difficult thing I am facing and have not yet overcome, is that I will not be able to carry another child. Diabetes is an auto-immune disease, thus resulting in patients being prone to more auto-immune diseases. My blood results are showing that I may have Lupus and this together with the Diabetes makes it far too great a risk to be pregnant.
Using a pump and how it’s changed my life, for better and for worse
I switched over to a Roche Accu-Chek Spirit Combo in 2013. I was originally on a different pump but I found the features and customer support for the Roche pump far outweighed the other brand. Having a pump is great! I was on 5 injections a day, so for someone who is needle phobic this is just awesome! The trickiest part is planning where on my body to wear the pump when I want to wear something without pockets, or for a day at the beach.
How I control my Diabetes
I must admit that I go through phases of control. I get demotivated really easily when it comes to strict control over my blood sugar levels. Life also gets crazy busy with a child, and so often the first thing that goes out the window is self-care, but he is also my biggest motivator for keeping and staying healthy.
My symptoms of hyperglycaemic or hypoglycaemic episodes
When my sugar goes too high I'll often get a headache along with increased thirst, fatigue, blurred vision and I find it difficult to concentrate.
When my blood sugar goes too low, I start sweating and get shaky and weak. My vision gets blurry as well and I also get a headache along with dizziness. I feel like my heart is racing and I get a feeling of anxiety and nervousness. This is also when I get grumpy and very moody or irritable. My hubby knows to just give me fruit juice and a snack.
My treatment for lows: usually a small box of fruit juice and then some pro vitas with cheese on works well for me.
Some of the other implications with Type 1 Diabetes
While I was pregnant, the blood vessels at the back of my eyes burst. I couldn't tell the difference between green and blue or pink and orange. If I lay down and suddenly got up I could see the blood floating around in my eyes and once it had settled there would be tiny black patches where I just couldn't see.
Other autoimmune diseases
I have tested positive on an ANA test. An ANA test detects antinuclear antibodies in your blood. Antibodies help you fight infection, but antinuclear antibodies attack your body's own tissues. Your body basically starts attacking itself. My main symptoms are that I am frequently tired, and my muscles and joints are sore.
Positive message for other Type One Warriors
I have to quote AA Milne here: 'Promise me you'll always remember: You're braver than you believe, stronger than you seem, and smarter than you think'.
There will always be challenges and obstacles that you need to face - but how you approach them and overcome them is what will define you and set you apart from others. Cands refers to those that are diagnosed with Type1 Diabetes as 'Type One Warriors', and I believe that that is because warriors don't get to rest - it's a 24 hour daily challenge. But with proper training (knowledge) and proper weapons (our team of doctors, dietitians, etc), and the correct armour (our medication) warriors come out victorious!
Lived with T1D for: 17 years
My diagnosis story
I was really sick. The previous year I had been diagnosed with bronchitis and from there I had started losing a lot of weight. I was 10 years old and looked like a rake. I remember going to see a friend of mine's gran in hospital one day and the lady lying next to her had diabetes. I didn't know anything about diabetes at the time but my friend told me that she was dying. Around the same time, my mom got really worried about my weight loss and took me to the doctor. He sent me off for blood tests and we went home.
I'll never forget that phone call at home: I answered the phone and it was the doctor. He asked to speak to my mom. We had another phone in my parents bedroom and she went there to talk to him. She started crying, and when she got off the phone she came and told me that I had diabetes and I needed to get to hospital.
I remember thinking about that elderly lady lying in hospital and I just started crying saying 'I don't want to die'. My blood glucose level was at 39, a non diabetic's ideal blood glucose level ranges from 4-6mmol/L.
I have a huge needle phobia so learning to inject myself and check my own sugars was a huge battle for me.
Dealing with Type 1 Diabetes in public as a child and teen
I have never necessarily been ashamed of being a Type 1 Diabetic, I’ve just never advertised it. When I was diagnosed the teacher at my school educated the class about diabetes. The friends I had were really supportive and most of these friends ended up attending the same high school as me so that adjustment was easy.
I met a friend on one of the diabetic camps and he would openly inject himself at the dinner table even through his jeans. I preferred to go away from people (usually the bathroom) to inject myself, but that was more because I was so afraid of people bumping me while I was injecting.
The most difficult thing to overcome being diagnosed a Type 1 Diabetic
Shew! I have found each phase of life has had such a different battle. Initially learning how to inject was tough. In hospital they taught me with a needle and an orange. Going back to school was also tough as I had missed a lot and trying to catch up was very stressful.
The pre-teen years were tough as we were still in the learning phase and adjusting medication. During my time of facing how to inject myself despite my fear, I went through what is known as the "honeymoon period'. This is when your pancreas kicks in a little and gives its last couple of squirts of insulin. Because my body was producing small amounts of insulin, the amount of insulin needed via injection was greatly reduced. I was starting to have hypos (episode of hypoglycaemia where your body has too little glucose going to the brain) but the doctor encouraged my mom to continue trying to get me used to injecting even if it was half a unit, or none at all.
My teen years were terrible. Hormones caused many issues for my sugars, often ending me up in DKA in hospital, and twice in a coma. With the added stress of exams and what to study or where to study - it was all just such a mess. Varsity was another challenge: the extra independence came with extra responsibility. Going out for drinks with friends wasn't as simple as just choosing what drink to have or whose house to have pre-drinks at. Clubbing, cocktails, shooters lead to late night/early morning burgers or feasts at the local clubs hotdog stand.
The next challenge was when I was pregnant. I had a terrible pregnancy. I was diagnosed with pre-eclampsia at 12 weeks and soon after I was diagnosed with hyper-emesis gravadium. My kidneys very quickly started showing signs of deterioration and I was battling terribly with my eyesight. My HbA1c was the best it has ever been in a long time when I was pregnant because of how disciplined I was - I had a strong motivation to be healthy. My baby was born at 26 weeks and this is the only time I have ever been grateful for my Diabetes. Diabetic women are known to have larger babies due to the excess sugar which in turn, makes the baby secrete extra insulin which then increases the fat deposits in the baby. My baby boy was only 300gms over the usual weight of a 26 week gestation baby, but any NICU mom will tell you that 300gms is a LOT!
To date, the most difficult thing I am facing and have not yet overcome, is that I will not be able to carry another child. Diabetes is an auto-immune disease, thus resulting in patients being prone to more auto-immune diseases. My blood results are showing that I may have Lupus and this together with the Diabetes makes it far too great a risk to be pregnant.
Using a pump and how it’s changed my life, for better and for worse
I switched over to a Roche Accu-Chek Spirit Combo in 2013. I was originally on a different pump but I found the features and customer support for the Roche pump far outweighed the other brand. Having a pump is great! I was on 5 injections a day, so for someone who is needle phobic this is just awesome! The trickiest part is planning where on my body to wear the pump when I want to wear something without pockets, or for a day at the beach.
How I control my Diabetes
I must admit that I go through phases of control. I get demotivated really easily when it comes to strict control over my blood sugar levels. Life also gets crazy busy with a child, and so often the first thing that goes out the window is self-care, but he is also my biggest motivator for keeping and staying healthy.
My symptoms of hyperglycaemic or hypoglycaemic episodes
When my sugar goes too high I'll often get a headache along with increased thirst, fatigue, blurred vision and I find it difficult to concentrate.
When my blood sugar goes too low, I start sweating and get shaky and weak. My vision gets blurry as well and I also get a headache along with dizziness. I feel like my heart is racing and I get a feeling of anxiety and nervousness. This is also when I get grumpy and very moody or irritable. My hubby knows to just give me fruit juice and a snack.
My treatment for lows: usually a small box of fruit juice and then some pro vitas with cheese on works well for me.
Some of the other implications with Type 1 Diabetes
While I was pregnant, the blood vessels at the back of my eyes burst. I couldn't tell the difference between green and blue or pink and orange. If I lay down and suddenly got up I could see the blood floating around in my eyes and once it had settled there would be tiny black patches where I just couldn't see.
Other autoimmune diseases
I have tested positive on an ANA test. An ANA test detects antinuclear antibodies in your blood. Antibodies help you fight infection, but antinuclear antibodies attack your body's own tissues. Your body basically starts attacking itself. My main symptoms are that I am frequently tired, and my muscles and joints are sore.
Positive message for other Type One Warriors
I have to quote AA Milne here: 'Promise me you'll always remember: You're braver than you believe, stronger than you seem, and smarter than you think'.
There will always be challenges and obstacles that you need to face - but how you approach them and overcome them is what will define you and set you apart from others. Cands refers to those that are diagnosed with Type1 Diabetes as 'Type One Warriors', and I believe that that is because warriors don't get to rest - it's a 24 hour daily challenge. But with proper training (knowledge) and proper weapons (our team of doctors, dietitians, etc), and the correct armour (our medication) warriors come out victorious!
My treatment regime
I have a Dexcom that continuously monitors my blood sugar. So every morning I wake up and look at my phone to see where my blood sugar is sitting. I then bolus according to what it is and what I'm going to be eating for breakfast. Lunch time is pretty much the same - check sugar, attempt to carbcount, bolus for the meal and eat. Throughout the day I check my phone to see what my blood sugar is doing. If my levels go out of range, my phone will alert me and I adjust accordingly.
The toughest part is the evenings for me. Having a little toddler to entertain, cook for, feed, bath and get into bed often sees my blood sugars taking a little dip. Paired with low blood sugar symptoms of irritability, anxiety, weakness and shakiness - it's just not fun. It's then supper time for us if we haven't eaten with our boy, and same routine as during the day. Then before I go to bed I give a little injection of some medication that helps prevent the extreme swing of lows and highs. If I wake up during the night I will often check my phone to see what my blood sugars are doing.
I use both insulin pens and an insulin pump. I originally was only using insulin pens and to get the closest to a 'functioning' pancreas, I found I needed to give 5 injections a day. This consisted of 1 long acting insulin in the morning (this covers me for 12 hours) as well as a quick acting insulin which will cover breakfast. Lunchtime is another quick acting insulin shot. Supper time is also a quick acting shot to cover the meal and then before bed it's one last long acting shot to see me through the night.
Not every day is the same as before - you can eat the exact same food one day as the next and do the exact same activity, but your body will throw in a surprise for you somewhere and you'll find yourself either having to give another shot or trying to correct a low blood sugar reading. I found the pump relieved a lot of this stress for me.
It’s annoying when people say things like “should you be eating that if you’re a Diabetic?”...
Oh my goodness, go and educate yourself please!!! I wish people would spend a little time learning about our disease and stop making silly statements like "should you be eating that?" or "You shouldn't be having that if you're a Diabetic".
Exercise
I don’t exercise. Should I exercise? Absolutely. I went through a phase where I was going to gym 3/4 times a week. Spinning class twice a week. Played tennis twice a week and danced (ballet) twice a week. I was exhausted every night, but my sugars were really well controlled and I got the most amazing sleep. Time is sadly not on my side these days.
Hardest part about being a Type 1 Diabetic
Lack of knowledge and education and lack of willingness to learn about this disease from others. I'm tired of explaining what I'm doing and why or what I'm eating and why. People don't always understand when you get tired - and I mean really tired (diabetic tired). Sometimes, because of the fatigue, I have to postpone get-togethers or change plans at the last minute.
Also, airport security is such a pain. So is trying to keep medication cool.
Best part about being a Type One Diabetic
I’m laughing out loud for this one - the best part for me was probably at school when I was having a low... I got to eat in class! But honestly, I really think the best part has been learning so much more about my body. Learning about this disease and helping others has been rewarding in itself. I've met so many amazing people because of this journey that I'm on.
One thing I’d love non-diabetics to know
The difference between Type 1 Diabetes and Type 2 Diabetes I guess. I always joke and say “my diabetes is nothing like your grandma’s diabetes”.
One thing I’d say to a newly diagnosed warrior
Set yourself goals. One goal can be to learn how to inject yourself, another can be learning to carbcount, another can be inserting a new infusion set for your pump etc. Having goals similar to these really helped me when I was diagnosed. It 'broke down' the trauma of being diagnosed, and each goal I accomplished felt like I was 'beating' it.
My support
My husband, Craig, is amazing. He knows what to do when I'm having a low or high, he knows how to help me correct it as well as what support and encouragement I need. My family is also wonderful. I think my diagnosis hit my parents hard and my mom has especially taken so much time to learn and do her best for me when I was growing up. I remember my mom and dad waking me up at 2am some mornings to see what my sugars were doing. I always woke up so grumpy, but even more so when my sugars were low. They would get me something to eat and while I was eating to get my sugars up my mom would rub my feet for me - instant good mood!
I have a Dexcom that continuously monitors my blood sugar. So every morning I wake up and look at my phone to see where my blood sugar is sitting. I then bolus according to what it is and what I'm going to be eating for breakfast. Lunch time is pretty much the same - check sugar, attempt to carbcount, bolus for the meal and eat. Throughout the day I check my phone to see what my blood sugar is doing. If my levels go out of range, my phone will alert me and I adjust accordingly.
The toughest part is the evenings for me. Having a little toddler to entertain, cook for, feed, bath and get into bed often sees my blood sugars taking a little dip. Paired with low blood sugar symptoms of irritability, anxiety, weakness and shakiness - it's just not fun. It's then supper time for us if we haven't eaten with our boy, and same routine as during the day. Then before I go to bed I give a little injection of some medication that helps prevent the extreme swing of lows and highs. If I wake up during the night I will often check my phone to see what my blood sugars are doing.
I use both insulin pens and an insulin pump. I originally was only using insulin pens and to get the closest to a 'functioning' pancreas, I found I needed to give 5 injections a day. This consisted of 1 long acting insulin in the morning (this covers me for 12 hours) as well as a quick acting insulin which will cover breakfast. Lunchtime is another quick acting insulin shot. Supper time is also a quick acting shot to cover the meal and then before bed it's one last long acting shot to see me through the night.
Not every day is the same as before - you can eat the exact same food one day as the next and do the exact same activity, but your body will throw in a surprise for you somewhere and you'll find yourself either having to give another shot or trying to correct a low blood sugar reading. I found the pump relieved a lot of this stress for me.
It’s annoying when people say things like “should you be eating that if you’re a Diabetic?”...
Oh my goodness, go and educate yourself please!!! I wish people would spend a little time learning about our disease and stop making silly statements like "should you be eating that?" or "You shouldn't be having that if you're a Diabetic".
Exercise
I don’t exercise. Should I exercise? Absolutely. I went through a phase where I was going to gym 3/4 times a week. Spinning class twice a week. Played tennis twice a week and danced (ballet) twice a week. I was exhausted every night, but my sugars were really well controlled and I got the most amazing sleep. Time is sadly not on my side these days.
Hardest part about being a Type 1 Diabetic
Lack of knowledge and education and lack of willingness to learn about this disease from others. I'm tired of explaining what I'm doing and why or what I'm eating and why. People don't always understand when you get tired - and I mean really tired (diabetic tired). Sometimes, because of the fatigue, I have to postpone get-togethers or change plans at the last minute.
Also, airport security is such a pain. So is trying to keep medication cool.
Best part about being a Type One Diabetic
I’m laughing out loud for this one - the best part for me was probably at school when I was having a low... I got to eat in class! But honestly, I really think the best part has been learning so much more about my body. Learning about this disease and helping others has been rewarding in itself. I've met so many amazing people because of this journey that I'm on.
One thing I’d love non-diabetics to know
The difference between Type 1 Diabetes and Type 2 Diabetes I guess. I always joke and say “my diabetes is nothing like your grandma’s diabetes”.
One thing I’d say to a newly diagnosed warrior
Set yourself goals. One goal can be to learn how to inject yourself, another can be learning to carbcount, another can be inserting a new infusion set for your pump etc. Having goals similar to these really helped me when I was diagnosed. It 'broke down' the trauma of being diagnosed, and each goal I accomplished felt like I was 'beating' it.
My support
My husband, Craig, is amazing. He knows what to do when I'm having a low or high, he knows how to help me correct it as well as what support and encouragement I need. My family is also wonderful. I think my diagnosis hit my parents hard and my mom has especially taken so much time to learn and do her best for me when I was growing up. I remember my mom and dad waking me up at 2am some mornings to see what my sugars were doing. I always woke up so grumpy, but even more so when my sugars were low. They would get me something to eat and while I was eating to get my sugars up my mom would rub my feet for me - instant good mood!
SLIMSY & TYPE ONE WARRIOR COLLABORATION GIVEAWAY
We have collaborated with Slimsy to offer our “type one warriors” an awesome giveaway. Be sure to like both of our Facebook pages, share a photograph with us on our Type One Warrior Facebook or Instagram page of a type one warrior that you know. Be sure to tell us a little bit about them and why they are your hero!
Sponsors & Prizes:
Type One Warrior: 5 limited edition, and the first of their kind, type one warrior t-shirts
Slimsy: 12 hampers containing 3 bottles of Slimsy's new Dairy Concentrate in Pina Colada, Orange and Berry Medley.
Competition closes on Friday, 24 November 2017.
Winner to be announced Monday, 27 November 2017
TERMS & CONDITIONS:
NO PURCHASE OR PAYMENT OF ANY KIND IS NECESSARY TO ENTER OR WIN.
The competition is sponsored by Slimsy and Type One Warrior. This contest is governed by these official rules. By participating in the contest, each entrant agrees to abide by these official rules, including all eligibility requirements, and understands that the results of the contest, as determined by sponsors and its agents, are final in all respects.
This promotion is in no way sponsored, endorsed or administered by, or associated with Facebook or Instagram. Any questions, comments or complaints regarding the promotion will be directed to the sponsors, not Facebook or Instagram.
ELIGIBILITY
The contest is open to legal residents of South Africa who have Internet access and a valid e-mail account prior to the beginning of the Contest Period. Sponsors have the right to verify the eligibility of each entrant.
COMPETITION PERIOD
The competition begins on 10/11/2017 and ends on 24/11/2017 at 23h59. All entries (submissions) must be received on or before the time stated during that submission period. Sponsors reserve the right to extend or shorten the contest at their sole discretion.
HOW TO ENTER
You can enter the competition via the Type One Warrior Facebook or Instagram page. Entrants must like the Slimsy and Type One Warrior Facebook pages and/or follow the Type One Warrior Instagram page, share a photograph of your type one warrior friend and a story explaining why they are your hero - share in the competition comments on the Type One Warrior page or tag us in your post on Instagram! After submitting the required information on the entry form, the entrant will receives one (1) entry into the drawing.
WINNER SELECTION
All eligible entries received during the Submission Period will be gathered into a database at the end of the Submission Period. Each sponsoring party will choose their top finalists and the winner will be announced on Monday, 27 November 2017. The announcement and instructions for the prize will be displayed on Facebook and Instagram. Each entrant is responsible for monitoring his/her Facebook or Instagram account for prize notification and receipt or other communications related to this competition. If a potential prize winner cannot be reached by Administrator (or Sponsor) within five (5) days, using the contact information provided at the time of entry, or if the prize is returned as undeliverable, that potential prize winner shall forfeit the prize. Upon the request of the Sponsor, the potential winner may be required to return an Affidavit of Eligibility, Release and Prize Acceptance Form. If a potential winner fails to comply with these official rules, that potential winner will be disqualified. Prizes may not be awarded if an insufficient number of eligible entries are received.
PRIZES:
5 Limited Edition shirts by Type One Warrior
12 Slimsy hampers containing the following 3 bottles of Dairy Blend
Incidental expenses and all other costs and expenses which are not specifically listed as part of a prize in these Official Rules and which may be associated with the award, acceptance, receipt and use of all or any portion of the awarded prize are solely the responsibility of the respective prize winner.
ADDITIONAL LIMITATIONS
Prize is non-transferable. No substitution or cash equivalent of prizes is permitted. Sponsor and its respective parent, affiliate and subsidiary companies, agents, and representatives are not responsible for any typographical or other errors in the offer or administration of the competition, including, but not limited to, errors in any printing or posting or these Official Rules, the selection and announcement of any winner, or the distribution of any prize. Any attempt to damage the content or operation of this competition is unlawful and subject to possible legal action by Sponsor. Sponsor reserves the right to terminate, suspend or amend the competition, without notice, and for any reason, including, without limitation, if Sponsor determines that the Sweepstakes cannot be conducted as planned or should a virus, bug, tampering or unauthorized intervention, technical failure or other cause beyond Sponsor’s control corrupt the administration, security, fairness, integrity or proper play of the competition. In the event any tampering or unauthorized intervention may have occurred, Sponsor reserves the right to void suspect entries at issue. Sponsor and its respective parent, affiliate and subsidiary companies, agents, and representatives, and any telephone network or service providers, are not responsible for incorrect or inaccurate transcription of entry information, or for any human error, technical malfunction, lost or delayed data transmission, omission, interruption, deletion, line failure or malfunction of any telephone network, computer equipment or software, the inability to access any website or online service or any other error, human or otherwise.
INDEMNIFICATION AND LIMITATION OF LIABILITY
BY ENTERING THE COMPETITION, EACH ENTRANT AGREES TO INDEMNIFY, RELEASE AND HOLD HARMLESS SPONSOR AND ITS PARENT, AFFILIATE AND SUBSIDIARY COMPANIES, THE FACEBOOK PLATFORM, ADMINISTRATOR, ADVERTISING AND PROMOTIONAL AGENCIES, AND ALL THEIR RESPECTIVE OFFICERS, DIRECTORS, EMPLOYEES, REPRESENTATIVES AND AGENTS FROM ANY LIABILITY, DAMAGES, LOSSES OR INJURY RESULTING IN WHOLE OR IN PART, DIRECTLY OR INDIRECTLY, FROM THAT ENTRANT’S PARTICIPATION IN THE COMPETITION AND THE ACCEPTANCE, USE OR MISUSE OF ANY PRIZE THAT MAY BE WON. SPONSOR AND ITS PARENT, AFFILIATE AND SUBSIDIARY COMPANIES DO NOT MAKE ANY WARRANTIES, EXPRESS OR IMPLIED, AS TO THE CONDITION, FITNESS OR MERCHANTABILITY OF THE PRIZE. SPONSOR AND ITS PARENTS, SUBSIDIARIES, AFFILIATES, ADVERTISING AND PROMOTIONAL AGENCIES, AND ALL THEIR RESPECTIVE OFFICERS, DIRECTORS, EMPLOYEES, REPRESENTATIVES AND AGENTS DISCLAIM ANY LIABILITY FOR DAMAGE TO ANY COMPUTER SYSTEM RESULTING FROM ACCESS TO OR THE DOWNLOAD OF INFORMATION OR MATERIALS CONNECTED WITH THE COMPETITION.
PUBLICITY
By participating, each entrant grants Sponsor permission to use his/her name, likeness or comments for publicity purposes without payment of additional consideration, except where prohibited by law.
COMPETITION SPONSORS
This competition is sponsored by:
Slimsy and Type One Warrior
Facebook links:
Slimsy - www.facebook.com/slimsy.juice
Type One Warrior - www.facebook.com/typeonewarrior
Instagram links:
Type One Warrior - www.instagram.com/typeonewarrior.co.za
Any questions regarding this competition should be directed to the Sponsors.
We have collaborated with Slimsy to offer our “type one warriors” an awesome giveaway. Be sure to like both of our Facebook pages, share a photograph with us on our Type One Warrior Facebook or Instagram page of a type one warrior that you know. Be sure to tell us a little bit about them and why they are your hero!
Sponsors & Prizes:
Type One Warrior: 5 limited edition, and the first of their kind, type one warrior t-shirts
Slimsy: 12 hampers containing 3 bottles of Slimsy's new Dairy Concentrate in Pina Colada, Orange and Berry Medley.
Competition closes on Friday, 24 November 2017.
Winner to be announced Monday, 27 November 2017
TERMS & CONDITIONS:
NO PURCHASE OR PAYMENT OF ANY KIND IS NECESSARY TO ENTER OR WIN.
The competition is sponsored by Slimsy and Type One Warrior. This contest is governed by these official rules. By participating in the contest, each entrant agrees to abide by these official rules, including all eligibility requirements, and understands that the results of the contest, as determined by sponsors and its agents, are final in all respects.
This promotion is in no way sponsored, endorsed or administered by, or associated with Facebook or Instagram. Any questions, comments or complaints regarding the promotion will be directed to the sponsors, not Facebook or Instagram.
ELIGIBILITY
The contest is open to legal residents of South Africa who have Internet access and a valid e-mail account prior to the beginning of the Contest Period. Sponsors have the right to verify the eligibility of each entrant.
COMPETITION PERIOD
The competition begins on 10/11/2017 and ends on 24/11/2017 at 23h59. All entries (submissions) must be received on or before the time stated during that submission period. Sponsors reserve the right to extend or shorten the contest at their sole discretion.
HOW TO ENTER
You can enter the competition via the Type One Warrior Facebook or Instagram page. Entrants must like the Slimsy and Type One Warrior Facebook pages and/or follow the Type One Warrior Instagram page, share a photograph of your type one warrior friend and a story explaining why they are your hero - share in the competition comments on the Type One Warrior page or tag us in your post on Instagram! After submitting the required information on the entry form, the entrant will receives one (1) entry into the drawing.
WINNER SELECTION
All eligible entries received during the Submission Period will be gathered into a database at the end of the Submission Period. Each sponsoring party will choose their top finalists and the winner will be announced on Monday, 27 November 2017. The announcement and instructions for the prize will be displayed on Facebook and Instagram. Each entrant is responsible for monitoring his/her Facebook or Instagram account for prize notification and receipt or other communications related to this competition. If a potential prize winner cannot be reached by Administrator (or Sponsor) within five (5) days, using the contact information provided at the time of entry, or if the prize is returned as undeliverable, that potential prize winner shall forfeit the prize. Upon the request of the Sponsor, the potential winner may be required to return an Affidavit of Eligibility, Release and Prize Acceptance Form. If a potential winner fails to comply with these official rules, that potential winner will be disqualified. Prizes may not be awarded if an insufficient number of eligible entries are received.
PRIZES:
5 Limited Edition shirts by Type One Warrior
12 Slimsy hampers containing the following 3 bottles of Dairy Blend
Incidental expenses and all other costs and expenses which are not specifically listed as part of a prize in these Official Rules and which may be associated with the award, acceptance, receipt and use of all or any portion of the awarded prize are solely the responsibility of the respective prize winner.
ADDITIONAL LIMITATIONS
Prize is non-transferable. No substitution or cash equivalent of prizes is permitted. Sponsor and its respective parent, affiliate and subsidiary companies, agents, and representatives are not responsible for any typographical or other errors in the offer or administration of the competition, including, but not limited to, errors in any printing or posting or these Official Rules, the selection and announcement of any winner, or the distribution of any prize. Any attempt to damage the content or operation of this competition is unlawful and subject to possible legal action by Sponsor. Sponsor reserves the right to terminate, suspend or amend the competition, without notice, and for any reason, including, without limitation, if Sponsor determines that the Sweepstakes cannot be conducted as planned or should a virus, bug, tampering or unauthorized intervention, technical failure or other cause beyond Sponsor’s control corrupt the administration, security, fairness, integrity or proper play of the competition. In the event any tampering or unauthorized intervention may have occurred, Sponsor reserves the right to void suspect entries at issue. Sponsor and its respective parent, affiliate and subsidiary companies, agents, and representatives, and any telephone network or service providers, are not responsible for incorrect or inaccurate transcription of entry information, or for any human error, technical malfunction, lost or delayed data transmission, omission, interruption, deletion, line failure or malfunction of any telephone network, computer equipment or software, the inability to access any website or online service or any other error, human or otherwise.
INDEMNIFICATION AND LIMITATION OF LIABILITY
BY ENTERING THE COMPETITION, EACH ENTRANT AGREES TO INDEMNIFY, RELEASE AND HOLD HARMLESS SPONSOR AND ITS PARENT, AFFILIATE AND SUBSIDIARY COMPANIES, THE FACEBOOK PLATFORM, ADMINISTRATOR, ADVERTISING AND PROMOTIONAL AGENCIES, AND ALL THEIR RESPECTIVE OFFICERS, DIRECTORS, EMPLOYEES, REPRESENTATIVES AND AGENTS FROM ANY LIABILITY, DAMAGES, LOSSES OR INJURY RESULTING IN WHOLE OR IN PART, DIRECTLY OR INDIRECTLY, FROM THAT ENTRANT’S PARTICIPATION IN THE COMPETITION AND THE ACCEPTANCE, USE OR MISUSE OF ANY PRIZE THAT MAY BE WON. SPONSOR AND ITS PARENT, AFFILIATE AND SUBSIDIARY COMPANIES DO NOT MAKE ANY WARRANTIES, EXPRESS OR IMPLIED, AS TO THE CONDITION, FITNESS OR MERCHANTABILITY OF THE PRIZE. SPONSOR AND ITS PARENTS, SUBSIDIARIES, AFFILIATES, ADVERTISING AND PROMOTIONAL AGENCIES, AND ALL THEIR RESPECTIVE OFFICERS, DIRECTORS, EMPLOYEES, REPRESENTATIVES AND AGENTS DISCLAIM ANY LIABILITY FOR DAMAGE TO ANY COMPUTER SYSTEM RESULTING FROM ACCESS TO OR THE DOWNLOAD OF INFORMATION OR MATERIALS CONNECTED WITH THE COMPETITION.
PUBLICITY
By participating, each entrant grants Sponsor permission to use his/her name, likeness or comments for publicity purposes without payment of additional consideration, except where prohibited by law.
COMPETITION SPONSORS
This competition is sponsored by:
Slimsy and Type One Warrior
Facebook links:
Slimsy - www.facebook.com/slimsy.juice
Type One Warrior - www.facebook.com/typeonewarrior
Instagram links:
Type One Warrior - www.instagram.com/typeonewarrior.co.za
Any questions regarding this competition should be directed to the Sponsors.
Last week we came home to a special delivery for Keto. A "Training" lead compliments of Friendly Dog Collar South Africa. Suddenly it feels official - our little Keto is well on his way to becoming Harrison's Diabetic Alert Dog.
Why is a lead like this important?
A lead that identifies your dog as a service dog, or one in training like Keto, is important because it lets people know without them having to approach the cute puppy that he is a working dog and shouldn't be interfered with.
I have had my eye on the leads for some time and was about to arrange with Row's family in the UK to please get a set for us to bring back with them when they return to South Africa. Luckily no such arrangements had been made.
Friendly Dog Collars has an amazing range of collars and leads that indicate to people the nature of their dog, such as "nervous" or "no dogs". Some examples below. They're reasonably priced for what they are and in South Africa there are slim pickings when it comes to this kind of dog apparel.
Visit their facebook page here.
I have had my eye on the leads for some time and was about to arrange with Row's family in the UK to please get a set for us to bring back with them when they return to South Africa. Luckily no such arrangements had been made.
Friendly Dog Collars has an amazing range of collars and leads that indicate to people the nature of their dog, such as "nervous" or "no dogs". Some examples below. They're reasonably priced for what they are and in South Africa there are slim pickings when it comes to this kind of dog apparel.
Visit their facebook page here.
Waking up this morning was hard. Waking up every morning is. We are exhausted beyond comprehension and we actually can’t even talk about how tired we are because we have no option of extra sleep, or sleeping in, or sleeping through our alarms.
22h00, 00h00, 02h00 - while the world sleeps we are checking our child’s sugar levels, fighting highs when he is high and fighting lows when he is low. No two nights are the same. No two nights are a given. There are just too many variables affecting a type one diabetic's levels. Every day and every night we fight for Harrison’s life. This is not an exaggeration, it is the truth.
We mind him with the eyes of a falcon. While he is so little our attention rests solely on him because yes, as Harrison’s parents we have to be selfish. We have to be for the simple fact that we are responsible for him. We are responsible for giving him the best care and the best chance at life as a normal child.
22h00, 00h00, 02h00 - while the world sleeps we are checking our child’s sugar levels, fighting highs when he is high and fighting lows when he is low. No two nights are the same. No two nights are a given. There are just too many variables affecting a type one diabetic's levels. Every day and every night we fight for Harrison’s life. This is not an exaggeration, it is the truth.
We mind him with the eyes of a falcon. While he is so little our attention rests solely on him because yes, as Harrison’s parents we have to be selfish. We have to be for the simple fact that we are responsible for him. We are responsible for giving him the best care and the best chance at life as a normal child.
Last week Monday, bright and early, we hit the road to Greytown to go and fetch our newest family member. A golden retriever, who we have named Keto, that we plan to train to become Harrison's Diabetic Alert Dog (D.A.D.). We did everything to make sure that we were prepared and ready. Below a checklist for any new pup owner with one or two extras for pups that are going to be trained.
These are the essentials:
These are the essentials:
| 1. Newspaper and rubbish packets, and lots of it. Keep it somewhere easily accessible for those accidents that need to be absorbed or picked up quickly. 2. Citronella, or even water, in a handy spray bottle for those naughty moments that call for a bit of discipline. Citronella has a strong smell that pups don't really enjoy so it also deters them from going back to continue their naughtiness. |
| 3. A good quality puppy food. In our home we are firm believers in feeding our dogs the best quality food that we can possibly afford, especially during the first 18 months. We have opted for the Ultra Dog Premium Large Puppy dog food. Jagger and Daisy, our older staffies, have been on Ultra Dog for several years now and for those who know our pooches know how active and agile they are. Ultra Dog Optiwoof sustains them and keeps them looking in peak condition. We couldn't think of any other food for our pup to start off on quite honestly. |
4. Sleeping arrangements: we have prepared the puppy crate with some soft bedding which, to start, will be placed in our kitchen at night. Once the pup has been properly potty trained we plan to move him next to Harrison's bed as this will be where he will sleep as he progresses through his training and grows up. We will eventually need to upgrade to a larger crate but whilst he is a puppy we are ok for a few months! We are opting for the crate method as this will become the pup's den so to speak. It will make travelling and transitioning to new environments easier as his one constant, his bedroom, will remain the same.
5. Chew toys and brain toys. As many different options as you can have available the better. Toys that can be filled with treats that can occupy the puppy for a period of time is great. The more challenging the better.
6. The previous owners were responsible enough to take their puppies in for inoculations and deworming and all that great stuff and this past Friday we took Keto in for his microchipping which is a prerequisite when you are putting your pets onto a medical aid (more on this next week).
Before we set about choosing our pup for Harrison we spoke to our friend, Adrienne Olivier, who is an accomplished dog trainer and GSD breeder based here in the KZN Midlands. She has seen us through the training of all of our dogs since 2005: Tara, Jagger, Madumbi, Daisy and Tata.
Asking Adrienne for advice in this field comes naturally, we respect her knowledge and experience so much. Save for packing her into our car and taking her with us, Adrienne equipped us with a list of things to assess in the choosing process. She understands our situation and gave us some pointers on how to choose the dog that would best fit in with our family and our need for a service dog whose job it will be to alert us for possible hypoglycaemic or hyperglycaemic levels.
We have decided to compile this list and document as much as what we can throughout this journey because we know that there are other families out there who might be in the same boat as us looking to self-train their own Diabetic Alert Dog because the cost of purchasing one already trained is just far too much.
Asking Adrienne for advice in this field comes naturally, we respect her knowledge and experience so much. Save for packing her into our car and taking her with us, Adrienne equipped us with a list of things to assess in the choosing process. She understands our situation and gave us some pointers on how to choose the dog that would best fit in with our family and our need for a service dog whose job it will be to alert us for possible hypoglycaemic or hyperglycaemic levels.
We have decided to compile this list and document as much as what we can throughout this journey because we know that there are other families out there who might be in the same boat as us looking to self-train their own Diabetic Alert Dog because the cost of purchasing one already trained is just far too much.
The checklist:
- The breed of pup is not necessarily important but you might prefer to find a breed that best fits your circumstances. Because Harrison is still so little we decided to choose a breed that is synonymous with an even temperament and has a great reputation with children and people in general. Had we been looking for just a pet we may have explored the option of rescuing a pup from the SPCA but the thing about a mix-breed, when you aren’t sure of the mix combinations, is the uncertainty of certain personality traits.
- Being purebred it often helps to know the bloodlines of the family so that you can check on the quality of the genes in that particular family. I have added this in here even though in our case this information is not available to us but you can get a fairly good idea by assessing the quality of the parents upon first meeting. If the information is available it will just equip you to make a better decision. These are the types of questions you can ask: “Have you registered this litter of pups?” - if no, “Are the parents registered?” - if no, “Were the grandparents registered?”... If the breeder has any information that can speak for the lineage you would be able to make a few calls to find out more about the quality of the dogs - things like no predispositions in the bloodline to hip dysplasia or other abnormalities are a great sign.
- Call the pups and see their reaction at the first meeting. We were standing a few feet away and called to the group of pups sitting around mom, every single one came running to us with their tails wagging. What a good sign! You want to choose a pup that shows a positive reaction. Avoid choosing the pup that hangs back from the group and doesn’t get in on the action.
- The surroundings are important too. Have a look at how the pups have been cared for by the owners of the dogs. The cleaner the better and you can see that they are being looked after well.
- For service dog training you are wanting a pup that is calm and confidant. Try not confusing a fearful pup with calm though. They need to present signs that they are socially attracted and interested in humans.
- Avoid the litter bully. THe little guy that is feisty and part of all the action, even instigating the action is probably not the best idea if you are wanting a pup that will listen and follow instruction without testing the limits too much. The litter bully will have a very strong temperament with high drive and will likely push the boundaries more than the calm confident pup. You want the middle of the road pup; the pup who isn’t fearful but also not too boisterous!
- Test the sound sensitivity of the pups by dropping a set of keys or clapping your hands. A positive response will be a pup who looks up and at the sound, even maybe motions towards the sound. A pup that scampers off and hides from the noise is not what you are looking for.
- Because labradors and golden retrievers have a reputation for mouthy-ness, while you might not get away with it completely you will need to find the pup that is a little bit mouthy but not a muncher. The pup that just has his jaws wrapped around everything is not the right fit, especially if you are wanting to train him to mind a young child.
- If you are getting your service pup for a young child, it best to take the child with and see the reaction of the pups to the child. Pups that show interest and are not afraid are good indicators that they have not been traumatised by other children and makes for a great relationship between them!
- One of the most important things to check, especially for Diabetic Alert Dogs is their retrieval drive. Have a piece of paper or something soft that you can rustle around and spark their interest. Tossing it away from you and seeing the pup follow after is a positive sign of a natural retrieval drive. Because your Diabetic Alert Dog will be trained to fetch your child’s testing kit it is better to have a dog that naturally wants to fetch things.
- Don’t rush the decision to get a puppy. It is a long term commitment and investment of time and energy so you really want to find the best fit for your family!